Managing Whiplash: Life After Injury
Whiplash is a general term for a mechanism of neck injury due to a rapid distortion of the cervical spine. It is frequently termed an acceleration and deceleration injury from the force that moves the head from one range of motion to another that is beyond the capacity of the anatomical structures to maintain equilibrium. Managing whiplash can be a minor rehabilitation and resolve or become a chronic, lifetime issue.
Although commonly involved in traffic collisions, about 1 in 10 cases of whiplash are due to injury from contact sports, falls and other accidents.The insulting motion involved may be complex, as in a side to side force, however, it is typically associated with being struck from behind. This involves a specific mechanism of injury where the lower neck is compressed from the head being thrown back in hyperextension, and the upper part of the neck is stretched from going forward into flexion.

The rapid movement resembles a whip as the weight of the head increases and subjects the cervical spine to excessive force. The resulting injury is often noted as sprain/strain of the neck. Technically, sprain involves ligaments and strain involves muscles, so this is a general, often initial working diagnosis. The resulting symptoms range from mild to severe, and are not always confined to neck pain.
Managing whiplash can be a simple process resulting in relief and recovery; or a complex problem that is controversial in nature due to frustration over resolution of symptoms and methods of treatment, to psychosocial issues and litigation ramifications associated with consequences suffering and/or incentives. Therefore, approximately half of whiplash injuries will result in chronic pain and disability.
Managing Whiplash Symptoms
The majority of symptoms from whiplash appear within a few days and are often limited to the neck area, consisting of pain and stiffness, however; there can be a multitude of symptoms that constitute a term called whiplash associated disorders:
- neck pain and stiffness
- pain in the arms, shoulders or shoulder blades
- headaches
- lower back pain that can radiate into the hips and legs
- dizziness, nausea and balance issues
- tinnitus or impaired hearing
- memory difficulties
- Jaw trouble or TMJ issues
- sensitivity to light, sound, touch, taste and smell
- symptoms from other body parts or organs, such as a stomach ache
- depression, anxiety and sleep problems
There are superficial and deep muscles as well as ligaments that stabilize the cervical which can be subject to eccentric stress, meaning stretched against constraint that can cause tears. If there is bleeding in these soft tissue, you may feel a lump that can make swallowing difficult for a few days.
Deeper structures like joints and surrounding soft tissues have sensory bodies that are important for balance and posture sense. This also includes vision and the inner ear’s balance organs. Disturbed signals from neck joints can cause problems with balance, as well as nausea and dizziness.
As pain becomes chronic you may become more sensitive to pain. Changes in nerve pathways can cause more soreness than usual and over-reaction to motion or muscle use can occur. Increased sensitivity of the nervous system can also cause stronger reactions to smells and taste. This increased nervous system sensitivity is usually called sensitization.
Recent evidence indicates part of this altered sensitivity is due to small fibre nerve pathology, which is a subgroup of sensory neuropathies that can cause sensory dysfunction at areas distant from the site of injury. In chronic whiplash, hand thermal and light touch detection were impaired, and heat pain thresholds were lowered.[1]
Fostering proper, early care and assurance can help minimize sensitization. Fear of motion is appropriate when justified and splinting of muscles can occur to help avoid damage from motion, however, early motion within limits helps reduce fear of motion which is beneficial to recovery.
Seeking Care For Managing Whiplash
If you have experienced a whiplash injury, you should contact your health care provider. If you are experiencing a lot of pain, get to emergency department. Seeking care as soon as possible is crucial; the sooner you are examined, the better care can be initiated in attempts at managing whiplash symptoms to reduce the likelihood of chronic problems, and the easier it will be to causally link symptoms to the mechanism of injury.
Documentation is crucial to proper management of therapeutic interventions as well as any medico-legal issues that arise. It is important a have a clear progression of events following sound clinical reasoning and appropriate behavioral response to avoid leaving issues to conjecture or inappropriate interpretation that confounds attempts at the best possible resolution outcome.
Initially, healing of tissues is important during the acute or inflammatory stage. A doctor may assess management at the early stage including determination for levels of activity. This is influenced by particular factors including level of injury and other complicating factors like previous injuries or conditions.
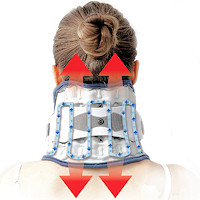 Neck Traction Devices Neck Traction Devices |
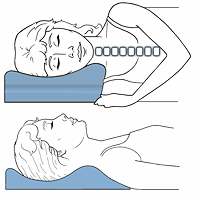 Functional Cervical Pillows Functional Cervical Pillows |
 Neck Support Collars Neck Support Collars |
Managing Whiplash – Pain Relief
Healing is dependent on blood circulation that is activated with movement. Small neck motions within limits and maintaining reasonable activities can foster early healing and relaxation beneficial to reduce psychological stress. Proper sleep allows better coping with pain and helps avoid memory difficulties.
Problems sleeping, anxiety, signs of depression, memory problems, difficulty concentrating, and other signs of post-traumatic stress should be addressed as early as possible. The main goal should be to avoid chronic issues. Complications may require a multi-disciplinary approach fostered through rehabilitation, pain clinics, and specialty whiplash management clinics.
Medications
Reducing pain is important to for early motion and proper sleep. Your doctor may determine any medications appropriate. Anti-inflammatory drugs like Ibuprofen or Naproxen can help with pain and inflammation. Medications for managing whiplash will vary from individuals. Medications may consist of pain killers, muscle relaxers and others. Some may be soothing, while others raise the pain threshold by affecting the nervous system.
Ice & Heat
Initially, ice packs can be used to help manage inflammation. This can be very therapeutic, especially in warmer climates.There are special ice packs that are anatomically designed to provide a more consistent application. If you are averse to icing, initially, heat should not be used as it can increase inflammation, however, a warm scarf in colder climates can help prevent muscle spasm due to chills. After a few days, heat applications can increase blood flow and relax muscles.
Supports
Supports like collars are often given to help reduce unwanted motions that may cause further injury. This will depend on the extent of the injury, level of stabilization, and range from rigid, more restrictive collars, to soft braces that can also help with temperature control. Soft braces can be soothing, can help with heat and ice applications, and should not be used just for show.
Tens
Another popular method of treatment is the use of mild electrical stimulation in the form of a tens unit (transcutaneous electrical nerve stimulator). This can help with home treatment and reduce dependency on drugs. Used on the skin, small electrodes can help reduce pain signals as well as help stimulate selected muscles, tendons and joints.
Therapy
As soon as possible, proper stretching and exercise is important to restore motion. This can focus on postural re-education to reduce strain on structures of the cervical spine that are prone to involved in chronic problems. Initially, basic motions are used to avoid overuse and possible insult and increased inflammation.
When there is global deficiencies in neck muscle endurance and perceived work ability, reduction of neck pain is greater with neck specific exercise compared to general physical activity.[2] Treatment must factor in a fear avoidance model: anxiety, followed by depression, fear, catastrophizing, self-efficacy, and consequential pain.
Specific neck exercise, particularly with a behavioral approach, can have a better impact on quality of life than general physical activity with chronic pain.[3,12] Considering chronic conditions display different variables of fear avoidance and perceived pain generators, variation from failed previous clinical trials is a reasonable approach.
However, even without a behavioral approach, specific neck exercises are particularly beneficial for those with neck pain and associated headaches. Almost 40% of those with chronic whiplash report ongoing headaches after 5 years, which makes it one of the most common persistent symptoms besides neck pain. These headaches are often associated with dizziness, and a new study found neck exercises to be beneficial, related mainly to physical and not psychological or sociological causes in this sample of patients.[4]
Recent reports indicate within 7 days following whiplash injury, neck pain was experienced by 84% and headache by 60%. At 12 months 38% of patients still experiencing neck pain, while 38% still reported headaches. While more clear definitions of and standardized reporting guidelines are necessary, it is clear that treatment should be geared towards preventing chronic, ongoing symptoms of headaches and neck pain.[5]
Chiropractic
Mobilization can be used early and within limits. Despite some medical recommendations to avoid Chiropractic care, Chiropractors may provide a very useful form of therapy and attempts to over generalize and/or marginalize ignores the fact that overzealous heath care providers are ill advised as excessive force can be used beyond physiological limits with exercise as well as manual and other forms of therapy.
I can tell you as a Chiropractor that I have seen countless patients over the years that have a chronic condition and have been through “the system”, only to be left with residual pain and problems. These are complicated cases and Chiropractors have built reputations on getting results when other methods have failed.
Managing whiplash involves consideration of complicating factors, patient specific needs, and attention to details within established protocols and when to amend these according to close attention to patient response is crucial to avoiding long term issues.
Therefore reassurance for issues like interference with daily life, concerns related to pain, psychological distress, and recovery is multifactorial and needs to be addressed in a nuanced manner and not just prescriptive.[6] Nuanced is defined as subtle shades of meaning or expression or done with extreme care to appreciate fine point distinctions.
There is often a failure to appreciate the pain producing generator in cases that have been essentially abandoned. These are often relegated to the ever popular and growing psycho-social aspects of ongoing pain. While this is justified in many cases and is often a part of the problem.
Often, to easily to forget is the fact that the term is bio-psycho-social and there may be a pain generator that has not been established and this should not be dismissed because it cannot be clinically detected or addressed by the practitioner’s means. Therefore, this pain generator or nociception relative to psychological factors is often underestimated.[7]
Managing Chronic Whiplash
Despite reasonable attempts, issues may not be resolved within a few months time. Improper care and healing can cause chronic pain and result in long term damage. Problems with excessive scar tissue in muscles can lead to chronic dysfunction as well as adhesions that can affect nerves. Improper ligament healing of ligaments and joints can lead to early onset of degenerative arthritis.
Changes in the spine over time may result in persistent symptoms, especially with instability of the spine and/or nerve damage. This may cause ongoing pain, headaches, and other symptoms of a nerve pain or chronic disc problems as a result of continued ongoing inflammation and instability.
Treatment for chronic symptoms may include counseling and behavioral interventions, more aggressive forms of physical or manual therapy, injections, and even surgery in some cases.
Risks for long term complaints are more likely among elderly, women, and previous cervical spine issues. Fear of movement is another risk for long term problems. Chronic whiplash management may include rehabilitation for mental and social situations, including aims to restore daily activities, including work.
Recent expert consensus recommended six main outcome domains for managing whiplash: Quality of Life, Pain, Physical Functioning, Work and Social Functioning, Perceived Recovery and Psychological Functioning.[8]
A new study proposes insurance company case managers may play a crucial role in rehabilitation of people with musculoskeletal disorders following minor motor vehicle crash injury.[9] Case managers were able to identify multiple factors including motivation and affect, communication, the role of lawyers, friends and family, geographic as well as cultural opportunities for more effective treatment.
Whiplash often results in soft tissue injuries to additional areas to the neck. A study indicates about 90% reporting injuries to other areas; 48% of reported shoulder pain, hand and wrist injuries are often suffered by drivers, knee injuries and other spinal areas. The greater number of body parts injured, the worse the psychological effect. The authors of the study concluded, “Our data confirm a strong association between these soft tissue injuries and psychological symptoms.”[10]
It can be difficult coping with a life that has changed as a result of an accident. Simple chores in everyday life, such as lifting objects, doing laundry, computer use, and even just spending time with friends and family can cause depression and perpetuation of pain. It may be difficult planning life from one day to the next. Finding different methods to manage pain and promoting as good a quality of life as possible is important. Caring health care providers and understanding loved ones plays a crucial role in managing whiplash.
Recovery in whiplash is often complex and has multidimensional elements. Additional factors to pain and disability, is the conceptualization of recovery which focuses on self-perception, emotional wellbeing, including cultural values and beliefs. Positive therapeutic attention to social and psychological influences is important in promoting recovery and wellbeing.[11]
 Using special imaging, it has been discovered that brain network dysfunction is correlated to fatty infiltration of the cervical muscles in chronic whiplash patients. The technique is called functional MRI and may indicate a need for this type of imaging in those considering the connection between disorder severity and neurologic changes.[13] The magnitude of fat infiltration in the medial deep cervical extensor muscles is significantly larger in those with severe chronic whiplash.[14]
Using special imaging, it has been discovered that brain network dysfunction is correlated to fatty infiltration of the cervical muscles in chronic whiplash patients. The technique is called functional MRI and may indicate a need for this type of imaging in those considering the connection between disorder severity and neurologic changes.[13] The magnitude of fat infiltration in the medial deep cervical extensor muscles is significantly larger in those with severe chronic whiplash.[14]
There are genetic components that also factor into chronic pain. Scientists have identified genetic factors that correlate with phenotypes associated with neck, shoulder, back, hip and knee pain. The genetic factors correlated to a biopsychological component of chronic musculoskeletal pain related to both psychological and physiological aspects of chronic pain processing and perception.[15]
 Muscle Therapy Tools Muscle Therapy Tools |
 Head Supports Head Supports |
 Special Pillows Special Pillows |
Using magnetization transfer (MT) imaging to quantify spinal cord white matter integrity, regional changes in integrity of whiplash patients after one year suggest potential insults to the cord. There was significant differences between males and females indicating worse outcomes in females.[16] Increased age, more injury severity and cervical spine degenerative changes indicate an increased risk for poor recovery and chronic symptoms.[17]
Managing Whiplash – Coping
The experience of self-management in chronic pain is one of fluctuating self-doubt, which is characterized by the perception of pain as a threat and low pain self-efficacy. During times of greater clarity, we develop strategies that increase pain self-efficacy and increase the perception of pain without threat. These are features of learning to live well with pain.[18]
Sometimes resolution is not possible. There are instances that suffering will be ongoing. This may result in resentment, especially in cases where one is not responsible for the injury, yet no compensation results. This is a frustrating result in some cases that alters one’s life in a tragic manner. One must remember that suffering is the default and no one is guaranteed a life of complete bliss.
I have been honored to know some of these individuals that serve as an inspiration, not only to me personally, but to others around them. Suffering with dignity and finding meaning under these circumstances is not the default, but is key to moving on and leading a meaningful life.
- “He who has a Why to live for can bear almost any How.”
– Friedrich Nietzsche
- “There is only one thing that I dread: not to be worthy of my sufferings.”
– Fyodor Dostoevsky
- “When we are no longer able to change a situation – we are challenged to change ourselves.”
– Viktor E. Frankl
References:
1 Eur J Pain. 2020 Feb 24
2. The Clinical Journal of Pain: June 05, 2019
3. Quality of Life Research. 2019 Feb
4. Medicine (Baltimore). 2019 Nov;98(48):e18130
5. Pain. 2020 Jan 16
6. Phys Ther. 2020 Apr 13
7. Curr Opin Support Palliat Care. 2019 Jun;13(2):94-98
8.The Clinical Journal of Pain: June 10, 2019
9. Disabil Rehabil. 2019 Aug 1:1-9.
10. Med Leg J. 2019 Dec 20:25817219875327
11. Clin J Pain. 2020 Mar 24
12. Sci Rep. 2020 Apr 21;10(1):6758
13. AJNR Am J Neuroradiol 2020 Jun 4.
14. Sci Rep. 2020 Jul 10;10(1):11471
15. Commun Biol. 2020 Jun 25;3(1):329
16. Sci Rep. 2020 Dec 17;10(1):22221
17. J Back Musculoskelet Rehabil. 2021 Aug 20
18. Phys Ther. 2022 Mar 30

