Cognitive Behavioral Therapy For Neck Pain
Cognitive behavioral therapy is a treatment approach that combines cognitive techniques, such as cognitive restructuring and thought-stopping, with behavioral techniques, such as role-playing and homework assignments which are applied to help acquire self management skills that enable one to recognize and modify bad thoughts and behaviors to reduce negative emotions and their contribution to pain, suffering, and functional disability.
 The cognitive behavioral therapy perspective is that therapeutic benefits are best achieved when patients believe the responsibility for action is theirs, perceive a successful outcome as the result of personal competence, and attribute the changes they are making to internal motivation rather than external pressure.
The cognitive behavioral therapy perspective is that therapeutic benefits are best achieved when patients believe the responsibility for action is theirs, perceive a successful outcome as the result of personal competence, and attribute the changes they are making to internal motivation rather than external pressure.
Treatment must therefore help patients to re-conceptualize their pain experience is changeable and to recognize that it is within their ability to relieve much or some of their pain and suffering. The goals are to provide the patient with the ability to monitor and identify the relationship between thoughts, feelings, behavior, and pain and to enable the patient to develop and implement more effective and adaptive ways of thinking, feeling, and responding.
As patients recognize their negative thoughts, the impact on pain, mood, and behavior becomes known and serves as to motivate change. For example, polarized thinking, seeing everything in terms of black or white, good or bad, can result in denying any improvement that is short of a total cure and can thus negate attempts to persevere and complicate further improvement.
Catastrophizing, a common negative thought pattern which produces emotional and physical reactions consistent with a worst-case scenario, unnecessarily worsening pain and anxiety. The goal is not to help solve a specific problem but rather to help the patient acquire a method that enables self management of dysfunctional thinking over situations.
Forms of irrational or negative thinking are presented and examined. Patients then monitor their thoughts in response to their pain and/or stress. Monitoring is accomplished by questions from the therapist (eg, “How did that make you feel?”) and later by patient journaling. Responses are then discussed in terms of the ABCD model, which stands for activating event (stressor), belief (resulting thought) about the event, consequence (emotions resulting from the thought), and dispute (examining the negative thought pattern that produced the negative feeling).
The patient is then helped to generate alternate ways of thinking about “A” that reduce negative emotional consequences (“C”). They are also directed in assessment of their behavior in response to their feelings and are helped to generate improved pain management options. Patients are taught numerous other cognitive techniques, including thought-stopping, which entails replacing the negative thought with pre-planned phrases, and benefit analysis, examining what hidden rewards contribute to maintaining the negative thought.
Behaviors may be influenced by the environment but also shape environmental events. It is important for pain patients to recognize and take responsibility for their potential influence on their environment, the distinction between control and influence being central. Individuals do not have the ability to control other individuals in their life, nor do they have the power to control most events. They do, however, have potential control over themselves, and by asserting control they improve the possibility of influencing both. Control does not mean curbing or restraining, instead it refers to communicating or behaving in a manner that increases the likelihood of eliciting the desired response or outcome.
 Neck Traction Devices Neck Traction Devices |
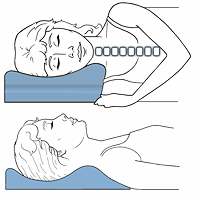 Cervical Pillows Cervical Pillows |
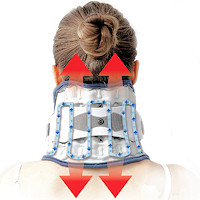
 Neck Support Collars Neck Support Collars |
Pain patients often have difficulty asserting themselves and communicate either passively or aggressively. Patients who are passive and avoidant lessen the possibility of affecting change in an aversive situation or interaction. Patients who explode often justify their anger as caused by their pain and then are surprised at the resentment and alienation with which others respond. Assertiveness and communication training is therefore an important part of the cognitive-behavioral treatment plan. Patients are given instruction and exercises in identification of passive, aggressive, and assertive responses to a variety of scenarios, the benefits of assertive versus passive or aggressive behavior becoming apparent.
The goals for cognitive behavioral therapy are for the patients to perceive themselves as having the ability and tools to manage their pain, will attribute effort to motivation, and success to personal competence. They will recognize that cognitions (thoughts) determine mood and behavior and will actively monitor and work to modify as needed the relationship between thoughts, feelings, behavior, and pain. Patients will seek to influence, rather than expect to control, their environment, through appropriate, assertive communication and self management.
So, you can seek a referral to a pain management specialist if you feel you need help in this area. Chronic pain is often associated with emotional difficulty, and rightly so. Cognitive behavioral therapy can be useful in these cases, as opposed to simply taking an anti-depressant. I think its important to go over this so one may gain some insight into the emotional aspects of pain and perhaps do some introspection and engage in dialog with others that might prove beneficial.
A 2018 study in the European Journal of Physical & Rehabilitation Medicine indicates it can be a beneficial form of therapy when combined with other methods like exercise. It is beneficial when a practitioner is familiar with some of these methods. It is not indicated for every patient and requires some extra time, but can be beneficial to include with therapy on some scale like in managing chronic whiplash, and to recognize when to refer.
The next part is Relaxation and Biofeedback for Neck Pain
Coping with Neck Pain | Education for Coping with Neck Pain | Relaxation and Biofeedback for Neck Pain | Active Adaptation for Neck Pain | Coping with Neck Pain Conclusion
