Knee Braces Are Used To Support An Injured Or Painful Knee
Knee braces can be used to protect the knee from injury or re-injury, limit motion and provide stability for healing after surgery or an injury and to remove weight from the joint. While some are used for warmth and mild support, others provide precise control with high levels of support and even reverse pressure from knee arthritis.

Almost 40 percent of injuries to the knee involve damage to ligaments. Most of these involve the anterior cruciate ligament. Due to neuromuscular, anatomical and hormonal factors, women suffer ligament damage more than men. A good functional knee brace provides the best stability and is an important part in managing recovery from these injuries.
Some of the more popular knee braces are sleeve types that slip on and are often made of neoprene. Depending on the quality of design, these can provide warmth, compression and increase position sense awareness. Generally, these are for more minor conditions or early stages of arthritis.
Because the knee is the strongest and largest of all the joints, bracing may require supports that offer significant mechanical advantage. Providing protection for demanding physical activities requires more than a simple sleeve.
Knee Braces For Arthritis
While there are many types of arthritis, osteoarthritis is a common problem of the knee. It is a progressive degenerative condition that is caused by wear and tear or overt trauma and often related to age. It can be caused by years of undue stress to the joint and can be a genetic factor. Regardless of the causes, it produces inflammation, instability, and pain. This pain can make everyday activities a challenge; things like walking or climbing stairs can be particularly troublesome as the joint gradually stiffens. Pieces of cartilage and bone spurs can cause the joint to lock up.
Braces are often used as part of a conservative therapeutic management for knee arthritis. The amount of support is usually related to the amount of degeneration, pain and instability. In cases where there is significant deterioration of the joint, the wearing of cartilage causes the bones to approximate and narrow, especially when weight bearing. This loading of the joint causes pain and further inflammation and damage. If the condition progresses to a point where the pain level is high and functional ability is deteriorated, surgery may be necessary for repair or replacement.
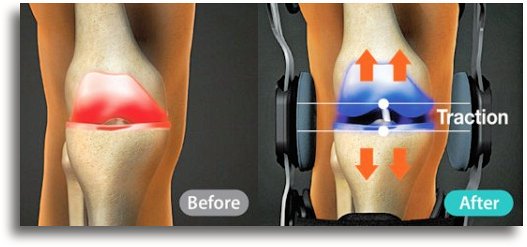
While pull on braces are very popular for early stages of arthritis, advanced conditions often respond well to unloading or traction type braces that work to decompress the joint. This can help reduce pain, increase ability to function and decrease medication use.
- A systematic review published in the 2011 American Journal of Physical Medicine & Rehabilitation found evidence that knee braces could be considered as part of conservative management for pain relief of pain, stiffness and increasing physical function for those with knee osteoarthritis.
- A 2013 study in the Journal of Musculoskeletal and Neuronal Interactions indicated there was evidence for beneficial effects of an unloading brace on both knee symptoms and biomechanics for those who have undergone surgery and subsequently developed arthritis.
- A 2015 study in The Knee Journal indicated a brace that unloads the knee for those with arthritis requiring surgery can improve knee related symptoms.
- A 2023 study in Current Rheumatology Reviews showed patients with knee osteoarthritis have impaired quality of life, especially in terms of physical activity and social functioning. Poor quality of life scores were associated with age, associated health issues (comorbidities), pain, function, as well as duration of disease.
Knee Braces For Muscle Weakness
Knee bracing may help in rehabilitation of weak muscles from a nerve injury, herniated disc or stroke. These conditions may alter the biomechanical aspects of walking allowing the knee to become unstable. A stabilizing knee brace can help provide support during rehab and in daily activities.
Braces can effect the sensory system allowing an improved feedback system and better knee control. A stabilizing brace can also help with motion training during daily activities as well as pain relief by preventing involuntary movement.
Knee & Back Pain
- A 2019 study in the Journal of Manual & Manipulative Therapy used MDT (Mechanical Diagnosis & Therapy) on patients with a primary complaint of knee pain that was non-acute. Using classifications of derangement for the spine and knee, they found almost half had a classification of spinal derangement of the lumbar spine.
- In a 2019 BMC Musculoskeletal Disorders found a relationship between lumbar degenerative disc disease and knee pain. Results indicated L1-L4 disc heights had a significant relation to knee pain, especially for L3 vertebral height and the medial or inside of the knee space.
Knee-spine syndrome is acknowledged in the scientific literature. Decreasing lumbar spine curve leads to increasing thigh muscle tension with knee flexion while standing, which can increase lower back pain and patellofemoral joint pain in the knee. Conversely, back pain symptoms may be caused or aggravated by degenerated changes in the knee. Those with flat back posture or loss of the normal lordosis display anterior or forward displacement of the center of gravity, creating instability and increases the biomechanical demands of walking and standing.
Sometimes the knee diagnosis is obvious; severe arthritis, ligament tears…, however; when there is a non-conclusive diagnosis with sub-acute or chronic knee pain, it is important to evaluate the musculoskeletal chain for related problems. The foot and ankle, as well as the hip and lower back can contribute factors in chronic knee pain. By addressing these as soon as possible, treatment can be more effective and more serious problems may be averted in some cases.
- A 2021 study in the Journal of Orthopaedic Science found that a tear of the medial meniscus posterior root can cause discomfort or a dull pain in the back of the knee (popliteal area) or the calf, which are sometimes misdiagnosed as sciatic nerve pain. These symptoms may indicate an impending ligament rupture or lead to arthritis or osteonecrosis. An MRI will show bone marrow edema from the meniscal root called a spreading roots sign may indicate the initial stage, while its disappearance was associated with acute rupture and the appearance of other MRI signs of posterior root tear like meniscal extrusion and giraffe neck signs.
Patella
- A 2020 study in the journal The Knee indicates an increase in lateral patellar tilt (LPT) can cause increased pressure on the lateral aspect of the knee and can lead to patellar or femoral cartilage damage and further osteoarthritis changes. For every 5 degree change om MRI axial imaging, related features, including cartilage and bone marrow lesions in addition to knee cartilage volume worsened on 2 year follow up. The measure is often used as a sensitive marker for indicator for patellofemoral instability syndrome.
The goal of treatment for patellar instability is achieving a pain free, stable and functional, knee as well as to ultimately to halt or slow the development of osteoarthritis. Non-operative treatment often consists of anti-inflammatory medications, a 3-6 period of immobilization followed by a progressive therapy regimen focusing on on range of motion, exercises, and vastus medialis obliquus strengthening, with adjunctive treatments such as knee aspiration and patellar stabilizing braces to decrease swelling and enable early range of motion.
- A 2021 study in Quantitative Imaging in Medicine and Surgery found that a higher position or outside tilt of the patella were associated with the development of iliotibial band syndrome, which is an overuse injury of the tissues on the outer thigh and knee.
- A 2021 study in the European Journal of Sport Science found that unilateral patellar tendinopathy causes postural balance of limb asymmetries and had increased rate of subsequent lower extremity musculoskeletal injury risk.
Useful Tips:
- A 2019 study in the journal Gait & Posture indicates a strategy for those with knee arthritis, demonstrating reduced medial compartment pressure by having the toe out foot position when standing from a sitting position. Depending on the extent and location of the arthritis, experimenting with toe in and toe out positioning may reduce pain and further damage.
- A 2020 Seminars in Arthritis and Rheumatism retrospective analysis on knee arthritis found that hyaluronic acid injections produced lower total medical care costs, fewer adverse events, with lower costs and use of prescription analgesics than corticosteroid injections and knee arthroplasty.
- A 2020 study in Biomed Research International found an association between foot posture and knee arthritis. The authors indicated when the feet are not symmetrical, this can lead to postural instability that effects the center of pressure and can significantly impact rehabilitation. Evaluation for wedge insoles to correct foot posture imbalance is important for knee problems.
- To make sleeping more comfortable, there are knee pillows and leg pillows that can help take pressure off the knees, especially when side sleeping. These products also help prevent lower back strain as well.
- A 2021 study in Ergonomics found high knee flexion postures like kneeling and squatting have been associated with increased incidence of knee injury. These are commonly adopted in childcare placing childcare workers at risk for knee health when caring for children of all ages.
- A 2021 study in the Journal of Orthopaedic Surgery indicates autologous plasma rich protein (PRP) injections for knee osteoarthritis led to a significant clinical improvement in middle-aged adults with a low to moderate knee osteoarthritis. BMI and higher arthritis grades were significant risk factors predictive for failure at mid-term follow-up.
- A 2021 study in the BMJ notes that topical diclofenac (an NSAID) seems to be effective and generally safer than oral drugs because of of reduced systemic exposure and lower dose related to side effects for long term use, and should be considered as first line pharmacological treatment for knee osteoarthritis.
- A 2021 study in the American Journal of Medicine repeated injections of corticosteroids plus hyaluronic acid more effectively decreased pain and improved physical function and physical functional performance than injections of hyaluronic acid alone from 1 week through 6 month.
- A 2022 study in Biomedicines found intra-articular injections of platelet-rich plasma (PRP) can provide clinically significant functional improvement for at least 6 months in patients with mild to moderate knee osteoarthritis, which is superior to hyaluronic acid (HA) and glucocorticosteroid (CS).
- A 2021 study in the European Journal of Pain concluded that transcutaneous electrical nerve stimulation or TENS provided evidence of immediate pain relief in individuals with mild to moderate knee osteoarthritis when TENS is applied along with functional activities, that usually induces pain.
- A 2021 study in Clinical Rehabilitation found TENS combined with other interventions was superior to other interventions for function in the medium term and long term. The authors conclude it could significantly relieve pain, decrease dysfunction and improve walking ability.
A 2022 study in Musculoskeletal science & practice confirms the best exercises for knee pain, specifically patellofemoral pain is combined hip and quadriceps strengthening exercises. This can be done easily and without strain for non-athletes.
- A 2022 study in the Journal of Sport Rehabilitation found Grade A evidence that mobilization with movement therapy is an effective method of treatment for reducing knee pain and increasing range of motion.
- A 2022 study in the American Journal of Translational Research found that joint injection of platelet-rich plasma (PRP) in combination with sodium hyaluronate can significantly reduce knee joint pain symptoms, improve knee joint function and reduce inflammation in treatment of knee osteoarthritis.
- A 2023 study in The Journal of Physical Therapy Science found osteoarthritis in older adults, rehabilitation aimed at achieving a smoother transition from sitting to standing can improve health-related quality of life and increase social participation.











