Degenerative Disc Disease – Normal Aging Or Disease Condition?
Increasingly, degenerative disc disease is viewed differently from the normal process of degeneration associated with aging. Factors involves, like genetics, environment, nutritional and disease factors, inflammation and the balance between tissue growth and death can play a role and effect individuals differently.
Degeneration originates from the latin word degeneratus, meaning no longer of its kind.

Is Degenerative Disc Disease Painful?
Neck and back pain is strongly associated with degenerative disc disease. The diseased state of disc degeneration is also associated with sciatica and neck disc herniation and back disc herniation. The process of degeneration alters disc height and the mechanics of the rest of the spine and may cause problems with other supporting structures such as muscles and ligaments.
The long term consequences are spinal stenosis (narrowing of openings that can place pressure on nerves and the spinal cord), which is a major cause of pain and disability. The incidence of degenerative disc disease is rising in the population and is the reason for over 90% of all spinal surgeries.
Studies have found that degenerative changes are noted in people without pain. This would not represent a diseased state and is an incidental finding on many x-rays and MRI’s. It may be that the process has not yet progressed to a disease state. Indeed, a 50,000 mile tire would show signs of wear and tear at 40,000 miles, however, at 20,000 miles, signs of the same wear and tear would not be considered “normal”.
It is important for health care practitioners to discern if findings on MRI’s are relevant to the objective and subjective assessments in order to avoid improper treatment. Likewise, it is important for health care providers to know when not to order special imaging studies to avoid misleading diagnoses. Because these studies are frequently ordered combined with many findings seen in asymptomatic populations, insurance companies are increasingly refusing to cover them, which can also lead to improper treatment. Seems financial incentives work both ways, all to the detriment of the patient.
- A 2015 study in the American J Neuroradiology using MRI on individuals 50 years of age and younger. The authors of the study concluded, “Meta-analysis demonstrates that MR imaging evidence of disc bulge, degeneration, extrusion, protrusion, Modic 1 changes, and spondylolysis are more prevalent in adults 50 years of age or younger with back pain compared with asymptomatic individuals.”
- A 2015 study in the Journal of Orthopaedic Science used a special MRI technique called T2 mapping to analyze degenerative disc disease and chronic low back pain. The authors of the study found a distinct correlation between chronic low back pain and degeneration of the back, outside part of the disc (annulus).
A major problem is that some individuals with MRI findings of degeneration suffer no pain; therefore, many call to eliminate MRI studies or downplay findings in those with pain. However, we know MRI findings are correlated with pain, especially Modic 1 changes of lumbar imaging, which is significantly correlated with pain.
- A 2018 study in the Journal of Pain Research found that, based on MRI findings, higher degrees of degeneration were found in those individuals with chronic back pain.
- A 2021 study in the European Spine Journal used multiparametric MRI contrasts extracted from Z-spectrum to determine painful from non-painful discs. This Z-sepctral MRI may prove to be a valuable tool in assessing symptoms related to parameters of degeneration causing pain like lower water content, collagen-bound water, collagen and lower pH.
The Process Of Degenerative Disc Disease
The disc sits between two spinal bones and consists of a soft nucleus (yellow) and firm annulus (blue) in the diagram above. A healthy disc acts like a water bed. There is a high water content in the nucleus and inner portion of the annulus which allows this portion of the disc to act as a fluid. The outermost part of the annulus acts as a skin or the covering of a water bed to restrain the inner portions. This creates hydrostatic pressure to reduce loading forces. Spinal discs have been described as shock absorbers, however, they are too stiff to perform this function and act to allow proper motion between spinal bones during movement.
 The main function of the disc is mechanical as it transmits load from body weight and muscle activity and provide flexibility, allowing bending (forward, backward and sideways) and rotation.
The main function of the disc is mechanical as it transmits load from body weight and muscle activity and provide flexibility, allowing bending (forward, backward and sideways) and rotation.
With increasing age, the water content of the disc decreases, forcing the disc to act more like a solid and resist mechanical loading in a haphazard manner as the hydrostatic pressure is reduced or lost completely. Injuries that affect the annulus or end plate can decompress the nucleus, and the healing process is taken over by severe degenerative changes.
The disc has little blood supply and cannot readily heal from injuries. Nutrition is through a process called diffusion where nutrients travel through the end plate (gray). The end plate is porous and permeable to allow the transport of nutrients. This permeability and the ability to transport nutrients normally decreases during growth and aging, however, it increases when there is disease due to disc degeneration and following end plate damage. This is one difference between normal aging and degenerative disease process. Additionally, nerve fibers normally only penetrate the outer area of the annulus, however, in degenerative disc disease, the nerves are noted to progress towards the nucleus and is associated with pain and inflammation. Back pain from the disc is usually started by physical disruption, and made worse or very painful by inflammation and low level disc infection.
 Load placed on a degenerated disc results in rapid loss of disc height and the joints behind the disc (facet joints) must change to bear the load which leads to arthritic changes. These changes result in what is called hypertrophy as there is a build up around the joints which may result in a facet syndrome and can narrow the spinal canal where the spinal cord runs through as shown in the diagram looking from above – down. The loss of height associated with degenerative disc disease can also reduce the tension on ligaments surrounding the disc causing loss of elasticity and bulging into the spinal canal, further narrowing the space for the spinal cord and leading to stenosis, as well as painful bending.
Load placed on a degenerated disc results in rapid loss of disc height and the joints behind the disc (facet joints) must change to bear the load which leads to arthritic changes. These changes result in what is called hypertrophy as there is a build up around the joints which may result in a facet syndrome and can narrow the spinal canal where the spinal cord runs through as shown in the diagram looking from above – down. The loss of height associated with degenerative disc disease can also reduce the tension on ligaments surrounding the disc causing loss of elasticity and bulging into the spinal canal, further narrowing the space for the spinal cord and leading to stenosis, as well as painful bending.
As the disc ages it becomes stiffer and weaker. Although degenerative changes can cause the annulus to collapse in some old discs, disc height does not show a major decrease with age. Severe disc degeneration cause a significant decrease in nucleus pressure and collapse of annulus height causing the disc to act like a flat tire. The disc height is important as it keeps the bones from placing pressure on sensitive nerves and loss of disc height can result in 50% of compression forces being transmitted to the joints behind the disc causing osteoarthritis in these joints as mentioned and diagrammed previous. The loss of disc height is also associated with similar type of osteoarthritic changes around the bones called osteophytes which attempt to stabilize the area.

Risk Factors For Degenerative Disc Disease
One of the highest risk factors for degenerative disc disease is genetic inheritance, accounting for in some estimates, over 70% in the lower back as well as in the neck. The primary factors associated with genetic influence related to degenerative disc disease is disc height and disc bulging. Stronger genetic effects are associated with earlier onset of degenerative disc disease.
- A 2014 study in the Journal of Occupational Rehabilitation noted that disc degeneration of the lumbar spine starts early in life and contributes to back pain development. The authors indicate significant risk factors for disc degeneration as: family history of degeneration, high level of sitting, back injury, bending/twisting, smoking, lifting, high physical workload, whole body vibration, and genetics. They additionally noted that the genetic risk factors were also associated with the severity of disc degeneration.
- A 2020 study in the journal Clinical Anatomy shows particular emphasis on the Vitamin D Receptor Gene or VDR gene and their polymorphisms. Previously indicated in a 2019 study in Scientific Reports, which also indicates relation to plasma levels acknowledging a genetic risk factor
- A 2021 study in the journal Spine found correlation of the Northeast US and significant variant-to-variant gene interaction to be associated with the risk of developing disc degeneration. The authors recommend corroborating and necessitating the inclusion of gene-gene interactions in predictive risk models. Gene-gene interaction or epistasis is the effect of one gene on a disease that is modified by another or several other genes.
- A 2016 study in Clinical and Experimental Rheumatology found an association of increased degenerative disc disease with Autoimmune thyroiditis, which often presents as hyper or hypothyroidism. The study included almost 8,00 patients and indicated one and a half times the rate of degeneration in those presenting with autoimmune related thyroid disease.
- A 2020 study in the journal Spine found lumbar puncture to be a risk factor for degeneration. A lumbar puncture or “spinal tap” is an outpatient procedure to remove some cerebrospinal fluid from the subarachnoid space of the spinal cord for testing. The risk was reduced with the use of image guidance during the procedure.
- A subsequent 2020 study in Clinical Neurology & Neurosurgery found lumbar puncture carries significant risk of penetrating the disc that and lead to accelerated joint degeneration. Total probability of disc penetration was 25%. A puncture can also be used to inject medicines for anesthesia and other procedures. Having it done guided seems to be a good idea.
- According to a 2016 study in the Journal of Orthopaedic Research, disc degeneration is a risk factor for disc degeneration! The authors found that increased levels of degeneration were found to produce the same amount of damaging altered motion in the disc adjacent to the one affected as in surgical fusion.
It has been a long term problem for surgical fusion as well as disc replacement, that the disc adjacent or next to the the one fused or replaced undergoes a more rapid degeneration. This is called adjacent segments disc disease. The authors of the study concluded, “Based on the current study it can be concluded that disc degeneration should also be considered as a risk factor in addition to fusion for generating adjacent disc degeneration.”
This shows the insidious and potentially damaging process of degeneration due to altered biomechanical and biochemical factors. This is influenced by genetics, work load, cumulative trauma and injuries.
- A 2020 study in the Global Spine Journal indicates caffeine may be a risk factor for degeneration especially with disc injury. Therefore, it may be a good idea to reduce or eliminate caffeine if you suffer an injury or have this condition.
- A 2021 study in European Cells & Materials found tungsten accumulates in the intervertebral disc and vertebrae stimulating disc degeneration and fibrosis as well as increase the expression of markers for pain.
Tungsten is used in many industrial goods, military applications and medical devices, however, emerging evidence has questioned the safety as studies have shown it can promote tumor formation, induce pulmonary disease and alter immune function. Although it is excreted from the body it can accumulate in certain organs such as the brain, colon, liver, kidneys, spleen and bones.
Characteristics Of Degenerative Disc Disease
Painful discs always show structural disruption and display irregular stress concentrations as the disc become sensitive to mechanical loading. The features most closely associated with pain include disc prolapse or herniation, loss of disc height, radial fissures, which are tears in the annulus that can leak fluid outside the disc lowering the pain threshold in surrounding tissues and internal disc disruption. Of these, loss of disc height is most closely related to pain history. Disc bulging and damage to the end plate which decompresses the nucleus are also associated with pain through a reactive process which allows blood vessels and nerves to grow into the disc, which is very painful.
Degenerative disc disease causes instability as the disc and surrounding tissues degenerate resulting in structural damage. This instability persists until the latter stages where fusion takes place. The instability causes increased and abnormal motion within the spine, however, movements become more painful, thus restricting overall motion.
In the neck, instability may be noted as intolerance to prolonged static postures, fatigue and inability to hold the head up, better with external support, including hands or a collar, frequent need for self-manipulation (cracking your neck), a feeling of instability, shaking or lack of control, frequent episodes of acute attacks and sharp pain, possibly with sudden movements.
In the lower back, the instability may present as diffuse, dull ache or a deep burning or sharp pain in the back, a feeling of weakness or an unstable back, pain may radiate to the hips or legs, and sitting intolerance – painful or discomfort when sitting.
Where significant disc height is lost, care should be taken during lifting and when exercising especially at the end range of motions like bending or twisting. Pain may often occur several hours after the actual damage to a disc that already has structural damage from degenerative disc disease. There may be pain free or minor discomfort during these activities, however, it may result in the inability to get out of bed the next morning. If there are reactive endplate or Modic 1 changes, activity can be painful and treatment resistant. Exercising, with Modic degenerative changes, despite being commonly prescribed for back pain, may be harmful this is very significant.
- A 2019 study in BMC Musculoskelet Disorders found that in a community of elderly individuals, loss of body height was most related to back pain. Disc disease is a major factor in reducing body height from loss of disc height. This factor was most associated with back pain over factors like body weight, fat, muscle, bone mass, smoking, chronic diseases, history of fall, and drinking habits.
The authors concluded, “It was suggested that postural changes in elderly people due to height loss and the causative disease may lead to LBP [low back pain] whereas postural changes due to LBP may also cause height loss.”
It is structural failure that predominates as an indication of degenerative disc disease. Structural failure impairing disc function does not occur as an inevitable consequence of age and is more closely related to pain. Structural failure is permanent because adult discs are not capable of repairing major defects. Because damage to one part of the disc increases the stress on other areas, the damage is likely to spread. Similar to a collapsed house, a physically disrupted disc can no longer perform it’s function even though the basic parts remain.
- The authors of a study in a 2008 European Spine Journal study indicated a healthy disc is intact structurally and has normal function and height, regardless of age. An ageing disc is intact structurally intact, has reduced function related to stiffening from the ageing process, but has normal height relative to age. A degenerated disc has structural failure and abnormal function, regardless of age. A disc that is completely degenerated has no signs of being normal. They further relate structural failure to the endplates.
- In a 2010 study in the journal Spine, the authors of this study indicate narrowing of disc space was more linked to back pain than osteophytes, and that narrowing of the disc space at 2 or more disc levels is more painful than narrowing at just 1 level.

In the above diagram you can see the effects of degeneration. A herniated disc can start the process; loss of disc pressure and height place excessive loads on the joints located towards the back. Increased load on the facet joints behind the spinal cord may cause hypertrophy or outgrowths of bone leading to a facet syndrome and/or joints in the back and side of the disc and in front of the spinal cord, which are called uncovertebral joints, may undergo the same degenerative process. Both of these, including herniations of the disc can lead to a pinched nerve or spinal radiculopathy.
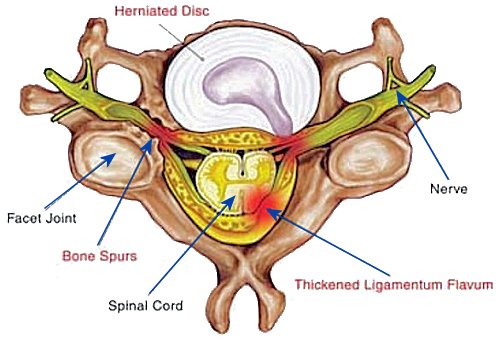
The image above continues to detail elements of pain related degenerative findings. The main focus of this picture is the ligamentum flavum or yellow ligament. Often noted in MRI findings as thickening or hypertrophy, this degenerative condition can cause narrowing of the space in the spinal canal. This is commonly referred to as spinal stenosis, but can be cause by a number of conditions. It basically means narrowing of the spinal canal, but stenosis refers to narrowing of an opening. Here we can see hypertrophy or thickening of the ligamentum flavum and the consequence of pressure on the spinal cord.
- A 2015 study in PLoS One Journal found a relationship between ligamentum flavum thickening and pain related to the degenerative process. Changes in this ligament can be inflammatory in nature and due to fibrosis or the accumulation of scar tissue.
- A 2011 study in the journal Spine found that thickening of the yellow ligament correlates with disc degeneration and the ligament can fold or buckle into the spinal canal due to degeneration more often than reactive hypertrophy. The authors, however, did not find a correlation with pain, but did find a significant correlation with disc herniation.
- A 2019 study in the Journal of Orthopaedic Research found that patients with spinal stenosis, especially women, had higher levels of pain from sensory hyperinnervation of the ligamentum flavum. The pain was related to increase pain nerve fibers in the ligament as opposed to strictly inflammation.
- A 2020 study in Orthopaedic Surgery outlines the many nerve fibers distributed on the ligament and the correlation with the mechanical characteristics and also indicated it may also be the anatomical basis of cervical vertigo.
Excessive mechanical loading or damage to the disc causes degeneration by disrupting its structure which causes a progressive and irreversible process resulting in further disruption. The combination of genetic inheritance and injury through too much or abnormal mechanical loading (or not enough) can weaken some discs to the point that physical disruption may follow a minor incident, such as a herniation following a cough or sneeze. Similarly, a tire made of inferior materials may rupture after hitting a small pothole in the road. As the foundation of a house weakens from deterioration, winds from a storm may cause failure or collapse.
- A 2009 study in the journal Spine indicates; “Patients who developed clinical symptoms during 10 years, including neck pain, stiff shoulder, and numbness in the upper extremities, demonstrated significantly more frequent progression of disc degeneration on MRI than those without the clinical symptoms.”
- A study in the 2009 Journal of Spinal Disorders and Techniques. 2009 May;22(3):214-8, indicates the normal response to loading of the disc is lost with degenerative disc disease, further supporting that structural damage leads to loss of function. The ability for a degenerated disc to resist normal loads and protect the sensitive structures of the spine is lost.
- A 2015 study in Clinical Biomechanics focused on the effect of degeneration of the spine on elderly patients and the risk of vertebral fractures. The authors of this study indicate that as the disc dehydrates, bone mineral density decreases, thus increasing the risk of vertebral fracture from falls. The authors call for disc degeneration to be included in the risk assessment for spinal fracture in the elderly. This can also be extrapolated to include those who have early degeneration or rapid erosive degenerative changes characteristic of Modic changes, regardless of age.
- According to a 2009 study in the Journal Spine, “The painful degenerative disc is significantly different from the asymptomatic degenerative disc with regard to histopathological findings”. The study indicated a strong expression of connective tissue growth factor expression in the painful disc related to disc fibrosis and degeneration. Painful discs showed chronic inflammatory reaction with blood vessel infiltration in varying degrees.
The annulus fibrosus had lost its normal architecture, and instead, disorganization, disruption, and crossed fusion were observed. The study further noted, “In other tissues, injury healing proceeds from the inside to the outside. On the contrary, healing in disc tissues proceeds from the outside to inside, since only the outer annulus fibrosus and longitudinal ligaments of discs possess vascular distribution. When the annulus fibrosus is lacerated or injured, vascular tissues can only gradually develop from the outer to the inner annulus fibrosus”.
- A 2015 study in the journal Spine indicated biomechanical data to show that continuous levels of disc degeneration in multi-level involvement exhibit higher frequency and severity of back pain symptoms compared to non-continuous, where non-degenerated discs were seen between degenerated discs.
The multi-level degenerated discs resulted in higher stress to joints, ligaments and bone than in the skipped levels involvement, even when the skipped level discs showed more degeneration. Therefore, a more consistent level of degeneration from one disc to the next presents higher biomechanical alterations resulting in more pain.
- An analysis in a 2015 American Journal of Neuroradiology article found that findings on MRI’s of degenerative changes were higher in those with back pain than without. Signs of disc degeneration showed about 2 times more likely to be associated with back pain, while disc extrusions and Modic 1 changes were about 4 times more associated with back pain.
- A 2020 study in Journal of Clinical Orthopaedics and Trauma investigated individuals with back pain and/or radiculopathy age 20 to 30 years old over a 9 year period. Of 730 patients, 58.6% had MRI evidence of degeneration, with 59.6% single level pathology and 41.4% multilevel involvement. While usually associated with older age, this study documents a high prevalence in pain associated changes in younger adults.
- A 2022 study in the International Journal of Environmental Research and Public Health indicates, “A reduction in disc height increases the likelihood of structural changes to the disc and bone-related changes.”
Problems With Degenerative Disc Disease
There is a certain type of degeneration which involves changes visible on MRI called Modic Type 1 changes, which have responded to antibiotics for back pain relief, as well as other therapies. This type of degeneration produces a deep type of pain that, may change in intensity, but is always there. It is usually most painful in the morning, better in mid afternoon, worse in late afternoon and worse at night. Pain on bending forward is problematic and it is not responsive to normal types of treatment, such as exercise. This may be related to an infection in the disc.
- A 2018 study in Emerging Microbes & Infections found that the bacteria Propionibacterium acnes induces intervertebral disc degeneration by promoting nucleus pulposus cell apoptosis (cell death), concomitant (associated with) with severe intervertebral disc degeneration. P. acnes was found to activate autophagy, likely to play a role in apoptosis of nucleus pulposus cells. Their findings further validated the involvement of P. acnes in the pathology of disc degeneration, providing evidence that P. acnes induced nucleus pulposus cell death is likely responsible for the pathology of degenerative disc disease.
- A 2018 study in Frontiers in Cellular and Infection Microbiology find an inflammatory cytokine interleukin (IL)-1β to be a key component of inflammatory responses to the bacteria P. acnes. Likewise, it is also involved in degenerative disc disease (DDD). The authors state, “Since there is a solid theoretical basis for this phenomenon, we further propose that the relationship between P. acnes infection and DDD is causal.”
- A study in the 2013 American Journal of Orthopedics indicates that disc degeneration of the lower back is found prior to hip joint degeneration and may actually help to cause osteoarthritis of the hip. In a related study in a 2013 edition of the European Spine Journal, a relationship was noted between loss of disc space at the L1/L2 and L2/L3 levels and hip pain.
- Mechanisms are outlined in detail in a 2013 issue of the European Spine Journal. As the spine undergoes the degenerative process in the discs and joints, the bones become remodeled and there is a weakening of the muscles, allowing a loss of the normal supportive curves. In the picture, you can see how degenerative changes cause an imbalance of the spine, resulting in a forward placement of gravity towards the hips (red circles). This could help explain the progression to hip arthritis with disc degeneration, as the entire body tries to compensate for spinal stiffens and muscle weakness.
The degenerative process can also produce sympathetic symptoms related to the neck which may include; headaches, vertigo, disequilibrium, tinnitus, scotomata, decreased vision, dysphagia, dysphonia, cough and anxiety. This is a condition known as posterior cervical sympathetic syndrome or Barre-Lieou Syndrome. It is a condition that is characterized by a host of cranial symptoms, such as headaches, abnormal functions of the eyes and the ears, and psychological and mental disorders. These are some of the symptoms usually not thought to be associated with neck conditions.
Dysphagia (difficulty swallowing) may be related to posterior cervical sympathetic syndrome and can be caused by factors related to degeneration like osteophytes – outgrowths of bone or other structures, as well as a condition called diffuse idiopathic skeletal hyperostosis (DISH).
- A 2015 study in the Journal of the Mechanical Behavior of Biomedical Materials outlined a study where the authors found that vertebral bones with osteoporosis are at increased risk for damage from compression where higher levels of disc degeneration is present. Disc degeneration weakens spinal structures; mainly the discs, facet joints, vertebral endplates and even the bone itself.
- A 2020 study in the Journal of Anatomy on disc degeneration found alterations in motion segment macro-mechanical function, disc matrix composition and cellular morphology. At the cartilage endplate bone interface, remodeling was observed coinciding with alterations in micro-mechanical properties and whole motion segment biomechanical parameters.
- A 2015 study in the journal Spine found that once the endplate is damaged or fractured, the disc becomes decompressed and loses it’s ability to resist forces. When bending forward, the average loss of pressure in the disc from endplate damage was 55%. This is very significant, however, the authors found that this alters the biomechanics of the spine and shifts weight bearing to joints that are not meant to resist force by 166%.
This sets up a situation that can result in degeneration and even effect the structure of the bone. This is seen in Modic changes, where endplate involvement leads to rapid degenerative changes and much pain when bending forward. Endplates keep the disc contained and they can be damaged by too much force like heave lifting.
There are 4 types of endplate lesions that are associated with disc degeneration as well as pain
- Schmorl’s nodes
- Fracture
- Erosion
- Calcification
- A 2019 study in the Journal of Orthopaedic Research found endplate defects were significantly related to disc degenerative scores, Modic changes, and disc displacement. The authors evaluated cumulative endplate defect scores which showed a strong association with back related disability.
- A 2020 study in PLoS One found that long periods of compression cause endplate degeneration and decrease vascular budding, which interferes with disc nutrition. This is an indication to avoid overcompression like sitting and altered postures like forward head, which increases compression. It further provides clinical reasoning for traction or decompression.
- A 2021 study in the European Spine Journal found disc degeneration determined a consistent reduction in the L5/S1 range of motion. As degeneration progresses, center of rotation were increasingly dispersed with no preference in direction.
- A 2022 study in Skeletal Radiology found traumatic endplate fractures are associated with accelerated disc degeneration and progression of segmental kyphosis in the thoracic and lumbar spine.
- A 2022 study in Nature Reviews Rheumatology found calcification is an often overlooked disc phenotype that cant have considerable clinical impact. It is not a rare finding, but is often ignored and under-reported. Calcification may lead to stiffer discs and altered biomechanics, more severe degeneration, inflammation and low back pain.
- A 2022 study in BMC Musculoskeletal Disorders found degeneration is associated with fatty infiltration of the multifidus seen on MRI, possibly due to inflammation. It is also associated with lumbar disc herniations.
Endothelial Dysfunction

- A hypothesis proposed in the 2015 journal Medical Hypotheses recognizes the genetic, individual and environmental factors of degenerative disc disease, however, they propose that endothelial dysfunction could be responsible for reducing nutrients to the disc, decreasing microcirculation and blood flow, leading to degenerative disc disease in the lumbar spine.
This theory emphasizes just how the disc receives its nutrient supply. The disc is not vascular; it has no direct blood supply and instead removes waste and receives nutrients through a process called osmotic diffusion from the small blood vessels that surround the disc and bone.
The continual stress from weight bearing compression in the discs of the lumbar spine is well known. This mechanical stress threatens the health of the discs in the lumbar spine by causing an imbalance in the endothelium, leading to reduced disc function.
Endothelial dysfunction is a systemic, not local, condition of the endothelium, which is located between the blood vessels walls and the blood stream and forms the largest organ in the body. It is responsive to mechanical factors like shear stress, pressure and hormonal stimulation. It responds by releasing chemicals that control blood vessel function, triggering inflammatory processes and affecting the normal balance or hemostasis. The authors consider this may be an early pathological cause of degenerative disc disease. Endothelial dysfunction has been linked to diabetes, kidney failure, peripheral artery disease and cardiovascular disease.
- A 2019 study in Osteoarthritis & Cartilage indicates degenerated disc nerves are mechanically sensitive and “deeply correlated” with the development of pain, representing a “decisive source” of low back pain.
- Smoking is thought to decrease microcirculation and is implicated in disc degeneration. A study in a 2014 Journal of Orthopaedic Research indicated that drugs can alter microcirculation, increasing or decreasing nutrient transportation, however, nicotine did not alter diffusion and produced an increase the number of vessels. It is also interesting to note that painful disc degeneration often involves what is called neovascularization, an increase in blood vessels in reaction to inflammation, and this causes an ingrowth of sensitive, painful nerve fibers.
- A 2020 study in JOR Spine notes “… vascular ingrowth into the cartilage endplates and inner layers of the annulus fibrosus is commonly associated with damaged or disrupted tissue, irrespective of age.”
Morning Back Stiffness
- A 2019 study in the journal Physical Therapy relates increased levels of lumbar degeneration to morning stiffness related to lower back pain. They noted an association between spinal morning stiffness and levels of radiographic evidence of decreased disc space an/or osteophytes.The significance was greater with increased levels of degeneration and longer duration of morning stiffness.
Degenerative Disc Disease & Inflammation: The Problem
 Painful disc degeneration results from many factors, however, inflammatory chemicals are produced with tissue damage. There are many of these, however, one of these chemicals is called tnf alpha (tumor necrosis factor-alpha). This inflammatory chemical is capable of producing pain by increasing the growth of sensitive nerve fibers into the disc.
Painful disc degeneration results from many factors, however, inflammatory chemicals are produced with tissue damage. There are many of these, however, one of these chemicals is called tnf alpha (tumor necrosis factor-alpha). This inflammatory chemical is capable of producing pain by increasing the growth of sensitive nerve fibers into the disc.
In the picture of a normal disc (top), nerve fibers are limited, mainly in the outer part of the annulus. (red & green – small nerves, brown – larger nerves). In the degenerated disc (bottom), nerves increase in number and depth, even going into the inner part of the disc, the nucleus pulposus.
These inflammatory chemicals are called cytokines, and they can cause destruction of tissues and pain. They increase with increasing severity of degeneration. These cytokines are very inflammatory. This highlights the importance of reducing inflammation as quickly as possible. An injury to tissues or disc herniation can release tnf alpha and this must be reduced. This brings into question the efficacy of spinal injections versus oral steroids. While injections of corticosteroids can more directly decrease inflammation, the process involves requires time, perhaps weeks, while an oral steroid like a medrol dose pack can be administered within hours.
- A 2003 study in the journal Spine used the drug infliximab to reduce the effects of tnf alpha in acute, severe inflammatory sciatica. For those with conditions that tnf alpha has an influence in a more chronic way like Modic changes, chronic disc herniation and nerve root irritation, drugs that are typically associated with chronic inflammation like rheumatoid arthritis or ankylosing spondylitis have been used with some success. Although these drugs can produce serious side effects like malignancy and liver damage.
The results of the study were impressive, 1 hour after infusion of the drug, leg pain reduced 50%. The improvement was noted after 3 months with significant reduction in leg pain and back pain related disability. There were no adverse reactions or effects of the drug.
- A 2015 study in the journal PLoS One indicates that tnf alpha can actually penetrate normal discs and remain for 4 to 8 days, even after the source of tnf alpha was removed. The tnf alpha caused damage and increased stiffness of the healthy discs. This may indicate that damage to surrounding structures can release tnf alpha into healthy discs and actually cause disc degeneration in addition to being part of the painful degenerative disc disease process.
The effects of altered structural integrity and biomechanical behavior were noted within 6 days. This is the structural disruption and consequences that differ normal age related degeneration from the frustrated healing of disc disease, where exposure to high levels of these inflammatory cytokines from inflammation or injury of spinal tissues rapidly breaks down disc structure and alters disc behavior.
Cytokines are involved with inflammation, however; there is another group of chemicals that are similar to cytokines called 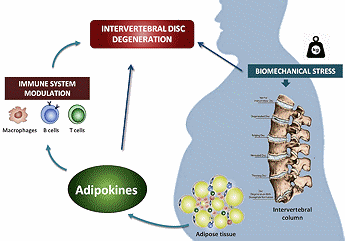 adipokines. Adipokines are produced by fat tissue and obesity not only increases mechanical forces in the spine, but produces inflammatory chemicals such as leptin, that is linked to degenerative and inflammatory processes.
adipokines. Adipokines are produced by fat tissue and obesity not only increases mechanical forces in the spine, but produces inflammatory chemicals such as leptin, that is linked to degenerative and inflammatory processes.
Obesity is known risk for low back pain and disc degeneration. Obese individuals have higher levels of serum leptin. Disc cells have receptors for leptin; therefore are susceptible to increased inflammatory responses, indicating a direct link to degenerative disc disease with unhealthy levels of fat tissue seen with obesity.
- A 2019 study in the European Spine Journal found leptin can initiate disc degenerative processes, especially with an existing environment of degeneration and inflammation, and indicates a biochemical link.
- A 2019 article in the International Journal of Molecular Sciences emphasizes the contribution of adipokines to chronic and persistent inflammation as well as the potential future for targets of therapeutic research. In the conclusion of the above extensive literature review, the authors conclude, “The available evidence summarized here, indicates that obesity, beyond mechanical action, exerts important metabolic and inflammatory effects on the homeostasis of intervertebral discs, which are mediated by adipokines.”
- A 2019 study in The Clinical Journal of Pain found inflammatory markers in both acute and chronic back pain, however, in both, there is an imbalance between anti-inflammatory and pro-inflammatory levels favoring production of inflammatory components.
Reducing Inflammation
What did I do? Without going into great details, I had an injury complicating my own severe disc degeneration complicated by multilevel Modic type 1 changes. I requested a medrol dose pack from my personal physician, however, he opted for injection. So, I had to see the orthopedist, get an MRI, then a prescription for the injection. Next, evaluation by the doctor doing and injection and scheduling for the injection. Well, I never made it to the appointment for injection evaluation. Why? It was weeks later and probably weeks more to go.
The inflammation was so painful and traveling upward, I considered a trip to the ER. Therefore, I had access to Bactrim, an antibiotic known for its anti-inflammatory effects on tnf alpha. Into the second day, the pain was 90% improved. This was not curative for my condition, nor a long term treatment, however, removing the inflammation in a rapid manner was very beneficial. I do not recommend this, always follow your doctor’s instructions.
Nonetheless, this emphasizes the importance of reducing inflammation in order to avoid further damage, especially in cases of existing disc disease. This also questions the use of initial pain relievers, muscle relaxants and typical anti-inflammatory medications, such as NSAID’s as well as untimely injection referrals in the use of injury or flare-ups related disc disease conditions.
- A 2015 study in the journal Lupus indicates supplementing with Vitamin D can reduce levels of tnf alpha. In the study, subjects took 4000IU per day and were able to reduce blood levels of tnf alpha by over 50%, and this correlated with a decrease in musculoskeletal pain. The subjects took Vitamin D3 in 1000IU softgels, 4 times per day.
- A 2015 study in European Review for Medical and Pharmacological Science found that curcumin can reduce inflammation and TNF-alpha levels and slow the disc degeneration process. Although this study was done on rats, an approach using the 4,000 IU of vitamin D and Curcumin is reasonable and easy to take in capsule form. The study did not find a difference between lower or higher doses of curcumin, so one quality capsule a day should suffice.
- To quote Dr. Akihiro Deguchi, in a 2015 article in the journal Endocrine, Metabolic & Immune Disorders – Drug Targets, “Thus, curcumin is one of the most promising phytochemicals that target various cancers and inflammation-mediated diseases”.
Along with reducing inflammation, it should be noted that diet can play a role. Certain foods trigger inflammatory chemicals, and a change in diet may help. Avoid fried, grilled and pasteurized foods, foods high in refined sugar, salt and preservatives, oils like corn oil with omega 6 fatty acids – instead use olive oil that has omega 3 fatty acids like fish or krill oil.
Sorry for the length of some of these articles, however, from some of your emails, I appreciate those who read, your kind encouragement, thought provoking questions, and the opportunity to help when I can.
- A 2021 study in Oxidative Medicine and Cellular Longevity found that tea polyphenols delayed the degeneration of nucleus cells in the disc by reducing oxidative stress, ultimately delaying the degeneration of intervertebral discs. Green and Black tea have the most polyphenols.
- A 2016 study in Anti-Inflammatory & Anti-Allergy Agents in Medicinal Chemistry indicates green tea has been demonstrated to have anti-inflammatory effects by suppressing the gene and/or protein expression of inflammatory cytokines and inflammation-related enzymes. The authors indicate “Since green tea and EGCG have multiple targets and act in a pleiotropic manner, we may consider their usage to improve the quality of life in patients with inflammatory disease.”
Degenerative Disc Disease & Death
- According to a 2015 study in the journal Arthritis & Rheumatology, there is an association between older men with severe disc degeneration and death from all causes. The authors also found an association between the severity of disc degeneration and calcification of the abdominal aorta. Well, this is not good news for those of us men with severe levels of disc disease.
Dealing With Degenerative Disc Disease
There has been a common belief among many health care providers that degenerative disc disease is just a part of normal aging and not relevant to any pain or disability that a patient is experiencing. This belief has led many to tell patients without any clear, traditional form of pathology to “learn to live with it” or “its all in your head”. This policy of nonintervention has not minimized the disability of neck or back pain and, in fact, perpetuates the very problems they desire to avoid. With a history of treatment drugs which have proven fatal and the high incidence of spinal surgeries performed for degenerative disc disease, it would seem unreasonable to suggest that chiropractic care, which has addressed this condition for many years, is not appropriate.
Mobilization, manipulation, massage, exercise, traction and posture modification are all reasonable therapies. Recently, TENS Unit Therapy has been shown to provide relief for degenerative disc disease. The major concern is progression of the disease to myelopathy.
If many methods have failed, you may look into Modic Antibiotic Spinal Therapy. If you visit this page, there is a questionnaire that may provide some insight as to if you might have Modic changes. While this is for back pain, because the studies have been focused on this, there is no reason to assume it does not produce similar findings in the neck.
You must remember that attitude is important. There is promising research being undertaken and things like antibiotic therapy, biological and genetic therapies.
- A 2019 study in the journal Pain found genetics plays an important role in factors which underlie disc problems. They found structural/anatomic factors as well as psychological components related to pain that demonstrate a complex genetic architecture related to lower back pain.
- A 2020 study in the journal Cartilage found 112 differentially expressed genes between the patients having disc degeneration and healthy controls which may contribute biomarkers for diagnosis and prevention, as well as seek new treatment methods to for repair/regeneration.
One must use reasonable means to break the chronic pain cycle as much as possible. You should not be afraid to perform reasonable activities and be comfortable within your limitations. Keep in mind that no two cases are the same and small things you can do can make a difference – you are not doomed to a life of severe, debilitating pain.
Some people will tell you your pain is psychological or due to depression. It is true that chronic pain is associated with depression, however, it seems reasonable to assume that a condition like degenerative disc disease, which does not improve and causes some degree of pain and/or disability, would be a cause for depression. However, this depression is not helpful and needs to be dealt with in coping with neck pain as well as back pain.
Chronic pain can form pathways in the brain that can continue pain sensation even when the pain generator is gone. This is called centralization and is being addressed through medications, however; lets make sure there is no pain generator before we write these patients off. Conditions like Modic 1 spinal degeneration are frequently written off as inconsequential, despite research indicating they are the degenerative finding on MRI most associated with pain, not responsive to traditional therapies, and made worse with exercise.
- A 2015 study in the Journal of Orthopaedic Science indicated tramadol-acetaminophen tablets to be effective for chronic low back pain, including degenerative disc disease, and it also provided the benefit of having an anti-depressant effect. The effect on depression was not experienced by those in the study who were instead given a non-steroidal anti-inflammatory drug. So, discuss medications with your doctor.
- In a 2014 study in the journal of Orthopaedic Surgery, they noted that there may be a significant relationship between metabolic syndrome and more severe cases of this osteoarthritic degeneration. Metabolic syndrome features central obesity (excess fat in the stomach area – apple shape), diabetes or high blood sugar problems, high blood pressure, and dyslipidemia (low HDL cholesterol or low levels of the “good cholesterol”).
- A study in the 2015 Journal of Orthopaedic Research indicates those with type 2 diabetes may be more prone to disc degeneration. They showed experimentally that type 2 diabetes discs have lower water and nutrient content as well as being stiffer and less elastic during compression.
 Remember that having a disc injury does not have to mean you had trauma like a fall or accident. We mentioned that the disc can get weak so that a sneeze can injure it. But injury to a disc means that it has been physically disrupted. This can happen from being weak, or from being overloaded as in lifting or from repeated small loadings that can become fatigued as the damage accumulates. If unexpected or sudden movement happen, internal muscle forces can cause injury, just like weakened and old spinal bones can fracture when just trying to open a window.
Remember that having a disc injury does not have to mean you had trauma like a fall or accident. We mentioned that the disc can get weak so that a sneeze can injure it. But injury to a disc means that it has been physically disrupted. This can happen from being weak, or from being overloaded as in lifting or from repeated small loadings that can become fatigued as the damage accumulates. If unexpected or sudden movement happen, internal muscle forces can cause injury, just like weakened and old spinal bones can fracture when just trying to open a window.
Professional help is certainly warranted if other methods fail or concern is great enough. Many drugs used today treat symptoms of chronic pain instead of specific pain generators. This is based partially on the fact that chronic pain can effect the brain, so if there is no pain generator that can be identified, the pain is still felt. This is like the phantom limb experience where there is no limb, but pain is still felt as if there were.
Another reason is that there is no belief that there is a pain generator. This is often seen with Modic changes which were long thought to be a normal part of the process of degenerative disc disease, but are now known to be highly associated with pain and disability. Modic Antibiotic Spinal Therapy is providing hope for this condition. Support of family and friends can help, however, you should not feel sorry for yourself or have other people feel sorry for you.
- A 2019 study in the journal Cells, Tissues, & Organs found that cortisol, a stress hormone, negatively contributes to disc degeneration and can be a perpetuating factor. We have talked bout stress in the tissues of the spine, however pain produces psychological stress and this can be detrimental to regenerative attempts.
Try to minimize drug dependency as much as possible. Be aware that fear of motion and activity is going to be a part of it. Similarly, depression and anxiety go hand in hand with chronic pain, especially when it limits your ability to function. A good doctor or therapist can help you and your family members understand and deal with this as best as possible. New discoveries are happening all the time. Old ideas regarding disc degeneration are changing. Try to keep hope, but get help if you need.
- A 2020 study in the International Journal of Molecular Sciences was able to show that the annulus cells of both mild and severely degenerated discs were able to respond to regenerative stimulation.
The annulus fibrosus part of the disc is crucial to disc integrity. Being composed of mainly consists of collagens and proteoglycans, they have a low turnover rate and very limited self healing potential. The results of the study are promising, and the the authors conclude, “These results give hope that regeneration of mildly but also strongly degenerated disc tissue is possible.”

Annular tears: a = peripheral tear or rim lesion; b = circumferential tear or concentric lesion; and, c = radial tear, a horizontal tear extending from the nucleus pulposus to the outer portion of the annulus fibrosus.
- A 2023 study in The Spine Journal indicates the annulus has limited capacity to heal and the repair process after injury is slow with continuous inflammation and cause further degeneration of the disc.
- A 2021 study in the Journal of Neurosurgical Sciences focused on injectable regenerative therapy using Mesenchymal Stem Cells (MSC) and Platelet Rich Plasma (PRP). All reported significant improvements in clinical and functional scores. No major complications nor adverse effects were reported. However, none of the studies reported a disc height improvement after treatment on radiographical outcome.
This implies a therapeutic benefit, however, further studies are needed to determine if these methods are truly regenerative.
Research into new therapies for treating degenerative disc disease is happening at a fast pace. Tissue engineering, genetics, biological treatment strategies, new drugs and surgical procedures are undergoing scientific trials. Sometimes, one is able to participate in these studies for new therapies. You can find out more at the clinical trials for disc degeneration.
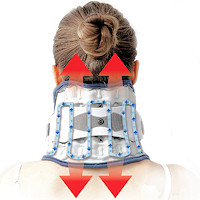 Neck Traction Devices
Neck Traction Devices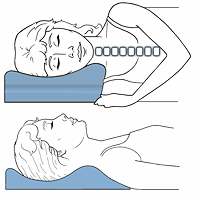 Cervical Pillows
Cervical Pillows Neck Support Collars
Neck Support Collars Traction & Inversion
Traction & Inversion Supports & Cushions
Supports & Cushions Belts & Corsets
Belts & Corsets Muscle Therapy Tools
Muscle Therapy Tools Head Supports
Head Supports Topical Pain Relievers
Topical Pain Relievers Special Pillows
Special Pillows Heat Therapy
Heat Therapy Cold Therapy
Cold Therapy Ergonomic Aids
Ergonomic Aids New Mattresses
New Mattresses Relief Supplements
Relief Supplements TENS Therapy
TENS Therapy Posture Braces
Posture Braces Neck Stabilization
Neck Stabilization