Back Herniated Disc Diagnosis & Treatment
Pain is a leading cause of work related back disability in people under the age of 45. Less than 15% will have an underlying nerve root problem related to a back herniated disc. The majority have a non-nerve back pain and most of these are assumed to be related to muscle or ligament injury or changes associated with disc degeneration. Despite this, little attempts are made to arrive at a specific diagnosis. Nonspecific diagnoses such as lumbar strain/sprain or lower back pain of unknown origin are very common.
Nerve pain related to a disc herniation is called radicular pain. Somatic pain is from a number of sources including muscles, joints and the disc itself. This can lead to confusion since pain patterns and symptoms may be similar. We will see if we can sort some of this out and make some sense of a pretty difficult situation.
Basic Disc Anatomy
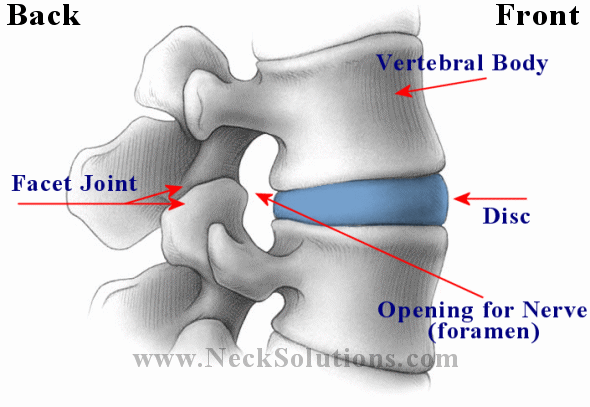
Lets take a look above at the basic anatomy of the disc and the vertebral unit. From the outside, you can see the disc, the top and bottom vertebrae (spinal bones) and the joints. The joints are the disc and its top and bottom vertebrae and the facet joints (2 on each side) in the back. While both joints are involved with motion, basically, the disc joint is involved in resisting compression, while the facet joints are involved with gliding. The back of the disc and the front of the facet joints form the foramen, which is an opening for the nerve that comes off the spinal cord.
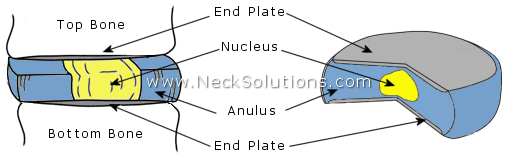
Taking it apart, you can see that the disc is made up of 2 parts; the annulus is the outer part in blue and the nucleus is the center part in yellow. You can also see the ends of the bones which go at the top and bottom of the disc have end plates, which are thin plates of cartilage.
What Happens In A Back Herniated Disc
A good analogy is comparing the disc to a jelly doughnut. The doughnut (annulus) and the jelly (nucleus). As we will see, the process of disc problems including herniations, are like the doughnut forming weak spots or tears from injury which allows the jelly to come out of place and push towards the outside of the doughnut. The jelly can bulge or protrude from the inside towards the outside or it can push all the way through the outside.

Looking from above down with the top vertebra (bone) removed, we can see a nice view of the disc and surrounding structures. The nerves come off the spinal cord, which runs down an opening called the spinal canal formed by the bones connecting together. The spinal cord continues up the spine and connects to the brain. As it it runs down the spine, spinal nerves come off at each level, forming a connection between the brain and every part of the body.
 To the left we see a herniated disc putting pressure on the nerve. Here, the nucleus (jelly) is pushing the annulus (doughnut) and the disc is herniated, protruding or bulging out enough to place significant pressure on the nerve root.
To the left we see a herniated disc putting pressure on the nerve. Here, the nucleus (jelly) is pushing the annulus (doughnut) and the disc is herniated, protruding or bulging out enough to place significant pressure on the nerve root.
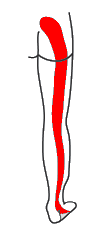
This causes not only back pain, but pain, numbness and tingling (paresthesia) in the area that the nerve runs to, often referred to as radiculitis. It can be in the hip region, into the thigh, leg and even into the foot. We will see the specific patterns that a herniated disc in the lower back causes for different levels of nerve pressure or pinching.
This can happen as a gradual process or all at once and can cause pain ranging from irritating to severe. Pain from a herniated disc referred down the leg is referred to as sciatica. There can be inflammation and muscle spasm as the muscles tighten to protect the sensitive nerves, often called muscle guarding.
We had mentioned the disc mainly resists compression forces, so the pain will be worse when there is more pressure on the disc. There can be pain when coughing, sneezing or straining. The pain will be worse when sitting, somewhat better when standing and not as bad when lying down. If you are holding an object, the pain will be worse the further out from the body and will be better the closer you hold it to your body – this is simple physics. Also, since the disc absorbs water, when you sleep at night, the pressure inside the disc is the greatest. Therefore, you should not do any heavy lifting when you first get out of bed as you are most likely to herniate a disc when the pressure is the greatest.
Types Of Back Herniated Disc
Terms used when describing disc herniations are often confusing. There is no simple way out of this. Different radiologists will use different terms depending on the sources of the information. A disc can be described as bulging, protruding, herniated, ruptured, prolapsed, extruded or sequestered; and further detailed regarding shape such as focal, localized or diffuse, generalized; or location as in central, medial (to the inside) or lateral (to the outside) of the nerve. Symptoms may vary differ depending on these variables. A “slipped disc” is not a technical term and provides no information. There can be an intravertebral herniation called a Schmorl’s node where there is a break in the vertebral body endplate. Some use terms related to the ligaments, like sub-ligamentous.
In general, the disc herniation is noted as contained – the nucleus within the contents of the annulus (jelly inside of doughnut) or non-contained – the nucleus outside the contents of the annulus (jelly outside the doughnut).

The above illustrates types of back herniated disc. You may agree or disagree and, in general, you are right either way. Again, it depends on the source used. Some consider a herniation to be a specific type of disc displacement. So, there is no uniform description of disc herniation that is used by everyone. Additionally, the symptoms vary; there may be a disc bulge with no pain and there may be a disc bulge that produces a lot of pain. Smaller, painful disc herniations may be more difficult to treat than larger, extruded herniations.
- A 2020 study in the Journal of Spinal Cord Medicine indicated that migrated or sequestered fragments from a disc herniation can cause persistent low back pain symptoms. The authors concluded, “Missed, migrated disc fragments can be implicated as a cause of low back pain, radiculopathy or cauda equina syndrome, especially in the absence of visible disc herniation. A high index of suspicion needs to be maintained in those cases with unexplained and persistent symptoms and/or no obvious disc herniation on MR images.”
A finding on MRI called Modic changes are associate with back pain. Specifically, Modic Type 1 changes are associated with a poorly healing back herniated disc and are, in some cases, indicative of a bacterial infection, which have responded to antibiotics for relief of back pain.
Internal Disc Disruption & High Intensity Zone
 One commonly overlooked source of chronic low back pain is internal disruption of the intervertebral disc. A disc can cause back and leg pain without involving the nerve root. This is disc mediated somatic pain as the disc is a potential pain generator. Internal disc disruption shows a loss of normal distinction between the nucleus and the annulus, disorganization and fissuring (tearing) of the annulus, a preserved external disc contour and appearance and absence of nerve root compression. The disc appears externally intact and undeformed on imaging but revealed painful annular pathology on discography.
One commonly overlooked source of chronic low back pain is internal disruption of the intervertebral disc. A disc can cause back and leg pain without involving the nerve root. This is disc mediated somatic pain as the disc is a potential pain generator. Internal disc disruption shows a loss of normal distinction between the nucleus and the annulus, disorganization and fissuring (tearing) of the annulus, a preserved external disc contour and appearance and absence of nerve root compression. The disc appears externally intact and undeformed on imaging but revealed painful annular pathology on discography.
Internal disc disruption is common; nearly 30% to 50% of subjects with chronic low back pain have internal disc disruption. A clinical diagnosis of internal disc disruption based on history and physical examination alone is extremely difficult. Most of the patients experience diffuse, dull ache or a deep seated, burning, lancinating pain in the back. Some will complain of a sensation of a weak, unstable back. Referral of pain into the hips and lower limbs is not uncommon.
- A 2020 study in Spine used weight-bearing MRI to detect behaviors between discs with outer, narrow and broad fissures, as well as within the posterior or back part of the annulus and between painful and non-painful discograms.
- A 2015 study in the International Journal of Clinical and Experimental Medicine indicates annulus tears, indicated on MRI by a high intensity zone (HIZ), cause high levels of inflammation responsible for back pain. The authors found that a disc with moderate levels of degeneration and a high intensity zone is diagnostic of a painful herniated disc.
- A 2014 study in the Chinese journal Zhonghua Yi Xue Za Zhi found that a high intensity zone on MRI located in the back (posterior) and bottom (inferior) part of the annulus part of the disc was common indication of disc disruption and significant when diagnosing back pain related to the disc (discogenic back pain).

- A 2015 study in Spine Journal indicated a high intensity zone was a risk factor for recurrent low back pain, being almost twice as likely to suffer another pain episode. The study also found higher levels of degeneration to be predicative of a future back pain occurrence. The authors further indicate the hazard for a future episode of back pain increases for each previous episode, noting the importance of MRI findings in predicting future risks of lower back pain episodes.
- A 2012 study in Annals of Physical and Rehabilitation Medicine reveals that individuals with severe acute back pain, without radiating pain or sciatica (axial back pain) were significantly more likely to have a high intensity zone on MRI.
- A 2006 study in the European Spine Journal indicates a high intensity zone is a reliable indicator of painful disc disruption of the annulus.
- A large scale 2020 study in the Spine Journal found these zones are relevant imaging biomarkers that are significantly associated with prolonged and severe low back pain and sciatica.
- A 2021 study in the Journal of Orthopaedic Research found a high intensity zone was associated with simultaneous presence of both Modic changes and end plate changes in the same motion segment.
Internal disc disruption is a common cause of disabling low back pain in a substantial number of young, healthy adults and repeated injury during active healing leads to persistent inflammation and enhanced disc degeneration of a pathological nature.
Modic Changes
A back herniated disc will typically heal and resorb in time, however, if the herniation pulls a piece of the endplate with it, healing can be complicated. This also opens a pathway for bacteria to enter the disc and subsequent modic changes due to infection, which complicates recovery with high levels of inflammation. Modic changes are associated with poor outcomes for herniated discs that become a chronic issue. This is an overlooked source of chronic and disabling back pain.
- A 2013 study in the journal Spine indicates that failure of the endplate junction is a common source of disc herniation. This break in the endplate not only allows for hernited disc material to extrude, but also provides a pathway for bacteria to enter, potentially causing infection associated with Modic changes. Endplate herniations contain cartilage and even pieces of bone and can complicate the recovery from a herniated disc.
- A 2015 study in the Global Spinal Journal shows that end plate damage causes decompression of the disc with associated disc height loss, and this can be caused by cartilage being pulled from the bone attachment. This can cause disruption of the intricate balance mechanism leading to degenerative changes and pose a risk factor for further damage.
Disruption of the endplate can be fracturing or herniation and may relate to Modic changes (lesion to the endplate and bone marrow) that is frequently associated with inflammation, especially type 1. Pulling off of the endplate may lead to the erosion often seen at lower lumbar spine levels that are associated with pain and degeneration. Pulling off of cartilage and the underlying bone can happen with acute (sudden) or repetitive (gradual) disc herniation, and pose a risk to healing through absorption.
- A 2023 study in bioRxiv indicates an endplate microfracture injury can induce Modic changes, disc degeneration and spinal cord sensitization.
- A 2021 study in the Journal of Pain Research found Modic changes were a strong factor, especially for the young, for recurrent lumbar disc herniation 1 year after endoscopic transforaminal discectomy. The authors indicate Modic changes reflect a reactive vertebral modification related to disc inflammation and an unstable microenvironment.
- A 2021 study in the Asian Spine Journal found endplate changes on MRI were associated with histological degeneration, inflammation and nerve infiltration in herniated discs. The authors indicate cartilage in the disc modulates degeneration and inflammation and indicates slow resorption and persistent clinical symptoms.
- A 2021 study in the European Spine Journal concluded the intensity of pain and disability in lower back pain is associated with the level of inflammation in the disc.
- A 2021 study in Clinical Anatomy found a direct correlation between separation of endplate cartilage and increased severity of disc herniation. The authors suggest the connection with endplate cartilage as an initiating link in the mechanical failure of intervertebral discs.
Signs Of Disc Related Back Pain
The above findings of high intensity zones and Modic changes are good indicators that the pain is disc related. These are often found in chronic cases on MRI. If these are missed, patients can be told it just in their head or just a normal part of the aging process. Specific pain generator indications can lead to additional or other methods of treatment. So, even with a herniated disc, some complicating findings can be missed. It may also be that a herniated disc is not the main source of pain.
- A 2017 study in Oncotarget, An Open Access Impact Journal, found reliable indicators of back pain due to disc problems. These problems may not present clinically as a typical disc herniation, but are related to disc damage, pain, and prolonged healing. These findings are High Intensity Zones and Modic changes, as discussed above. However, lets re-visit this for a moment, so it is clear and concise.
A High Intensity Zone (HIZ) seen on MRI is significant when seen in the posterior or back of the disc. It is fluid/mucoid material with new blood vessels and granulation tissue encased between torn fibers of disc annulus or under the posterior longitudinal ligament that runs along the back of the discs. They result mainly from mechanical loading fatigue, as well as inflammation due to repair of a disc tear. Now a disc tear represents not only mechanical injury and inflammation, there is also a means for bacteria to enter in this special non-aerobic environment, thus providing conditions for a low grade bacterial infection as seen with some Modic changes. “So we conclude that HIZ on T2-weighted MR images is credible to forecast the discogenic LBP.”
Modic changes show as signal abnormalities on MRI in the bone marrow of the associated disc. These lesions of the endplates are confirmed to be associated with back pain from the disc. Modic changes are an accelerated form of disc degeneration that can go into the nucleus of the disc, beyond the annulus or outer part. Modic changes show a high diagnostic significance for disc related (discogenic) low back pain. “The results conducted by our research confirmed the association between the discogenic LBP and Modic change.”
- A 2016 study in PLoS One found 5 questions were useful in diagnosing disc related low back pain related to degeneration. A positive response of pain to 3 – 5 of the questions was indicative of degeneration related discogenic pain:
- After sitting too long
- While standing after sitting too long
- Squirming in a chair after sitting too long
- While washing one’s face
- In the standing position with flexion (bending forward)
- A 2020 review in the International Journal of Rheumatology indicates disc pain is usually felt in the lumbar spine region and may be felt in the buttocks, down to the upper thighs. Radicular pain or pinching of the nerve usually presents with muscular weakness and sensory problems in the distribution of the buttock, lower abdomen, groin region, and lower extremities. There can be both involved.
Findings Of A Back Herniated Disc
The assessment is based on history and physical examination which includes neurological examination, motor examination, sensory examination, reflex examination, and application of provocative maneuvers or orthopedic tests. This represents a more classic or textbook example of a herniated disc.
| Disc Herniation | L3-L4 | L4-L5 | L5-S1 |
| Nerve Root | L4 | L5 | S1 |
| Pain |  |
 |
 |
| Low back, hip, front/side thigh, inside leg | Above SI joint, hip, side thigh and leg, top of foot | Above SI joint, hip, back side thigh and leg, heel | |
| Numbness |  |
 |
 |
| Front inside thigh and knee | Side leg, first 3 toes | Back calf, side leg, heel and toe | |
| Atrophy – wasting | Quadriceps | Minor | Gastocnemius, soleus |
| Motor weakness | Extension of quadriceps | Dorsiflexion (pull up) great toe and foot (foot drop) | Plantar flexion (push down) great toe and foot |
| Screening exam | Squat and rise | Heel walking | Walking on toes |
| Reflexes | Knee jerk diminished | None | Ankle jerk diminished |
Sometimes, there will be a position that will make the pain worse or better, depending on the location of the herniated disc. Below is graphic which shows how a disc herniated medial (inside the nerve root) or lateral (outside the nerve root) can cause a person to assume a certain position called an antalgic lean.
As you can see, by examining which way a person with sciatica from a herniated disc leans, you can get an indication where the herniated disc is in relation to the nerve root.
Radiation of pain needs to be carefully interpreted. Somatic referred pain in the buttock or lower limb can be expected. Somatic referred pain is mostly in the buttock or lower extremity without any type of pain generators in the back and it should not be confused with radicular pain from a nerve root. The differences are in the quality of pain and its behavior. Below you can see the differences between radicular pain from a back herniated disc and somatic pain.
| Somatic or Referred Pain | Radicular Pain | |
| Segment Causes | Posterior segment or element | Anterior segment |
| Facet joint pain | Disc herniation | |
| Sacroiliac joint pain | Annular tear, discogenic pain | |
| Myofascial syndrome | Spinal stenosis | |
| Internal disc disruption | ||
| Symptoms | ||
| Dull, aching, deep | Sharp, shooting, superficial, lancinating | |
| Like an expanding pressure | Like an electric shock | |
| Poorly localized | Well localized | |
| Covers a wide area | Leg worse than back | |
| Back worse than leg | Paresthesia present | |
| No paresthesia | Well defined | |
| No radicular or shooting pain | Radicular distribution | |
| Modification | Worse with extension | Worse with flexion |
| Better with flexion | Better with extension | |
| No radicular pattern | Radicular pattern | |
| Radiation | Low back to hip, thigh, groin | Follows nerve distribution |
| Radiation below knee unusual | Radiation below knee common | |
| Quasi segmental | Radicular pattern | |
| Signs | ||
| Sensory Alteration | Uncommon | Probable |
| Motor Changes | Only subjective weakness | Objective weakness |
| Atrophy rare | Atrophy possibly present | |
| Reflex Changes | None | Commonly described, but seen only occasionally |
| Straight Leg Raises | Only low back pain | Reproduction of leg pain |
| No root tension signs | Positive root tension signs | |
| Adapted and modified from: Manchikanti L, et al. Low back and lumbar radicular pain. In: Manchikanti L, et al (eds). Clinical Aspects of Pain Medicine and Interventional Pain Management: A Comprehensive Review. ASIPP Publishing, Paducah, KY, 2011, pp 87-114 (374). | ||
Chronic, persistent low back, lower extremity pain, and radicular pain may be secondary to a back herniated disc, disc disruption, disc degeneration, spinal stenosis, or after surgery resulting in disc related pain with or without radiculitis. There is much information regarding cause, diagnosis, and numerous treatment methods for herniated disc pain. As we have noted, magnetic resonance imaging (MRI) findings of a herniated disc are not always accompanied by symptoms.
The prevalence of a symptomatic herniated disc in the lower back is about 1% to 3% with the highest prevalence among people aged 30 to 50 years, with a male to female ratio of 2:1. In individuals aged 25 to 55 years, about 95% of herniated discs occur in the low back called the lumbar spine at the L4/5 and L5/S1 levels; disc herniation above this level is more common in people aged over 55 years and upper lumbar disc herniation may be associated with hip pain and/or groin pain. Disc displacement may present as internal disc disruption, disc prolapse, disc protrusion, disc extrusion, disc herniation, or simply discogenic pain. The estimated prevalence of lumbar radiculopathy or sciatica has been described as 9.8 per 1,000 cases, 5.1 in men and 3.7 in women.
Irritation of the nerve root (lumbar radiculopathy) from a herniated disc resolves by itself about 23% to 48% of the time, but up to 30% to 70% will still have significant symptoms after one year, with 5% to 15% requiring surgery.
It should be noted that one sided lower abdominal swelling may be a presentation of an upper lumbar disc herniation. This may been seen with burning sensation in the front/side aspect of the thigh caused by a lateral L2-3 herniation.
- A 2013 article in Case Reports in Orthopedics notes that thoracic disc herniation can result in pain, sensory disturbances, myelopathy, and lower extremity weakness. They also noted extraspinal complaints, such as gastrointestinal or cardiopulmonary discomfort. The authors concluded, “Therefore, TDH [Thoracic Disc Herniation] should be included in the differential diagnosis of patients with negative gastrointestinal, genitourinary, and cardiopulmonary system basic studies.”
 |
 |
| Central Canal Stenosis | Lateral Recess Stenosis |
Stenosis
The term stenosis means narrowing of an opening. This can be at the foramen where the nerve runs through or spinal stenosis, which is narrowing of the spinal canal, resulting in symptoms and signs caused by compression of the vascular and nervous structures. Disc bulging, protrusion, and herniation combined with degenerative bone growth called osteophytes and changes of the facet joints can cause a narrowing of the spinal canal. Central spinal stenosis is prevalent in about 27.% of the population.
Symptoms of central spinal stenosis may be related to arterial flow, venous congestion, and increased pressure; the nerve roots can be irritated by local inflammation; or direct compression in the central canal. Spinal stenosis is a disorder related to many factors, and symptoms can vary with or without pain in the buttocks or legs when walking, which disappears with sitting or lower backk flexion (bending forward) and this is called neurogenic claudication.
- A 2020 study in Biomed Research International found that stenosis with claudication leads to a forward bent walking position and foot pressure measurements indicates risk of falls forward and to the symptomatic side in the elderly.
Central spinal stenosis resulting in radiculopathy is differentiated by pain on walking that is relieved by rest, the feeling that the legs are going to give away, a feeling of cold or numbness in the legs, a feeling that the legs are made of rubber and do not belong to the patient, and night pain that is relieved by walking. In addition, radiologic evaluation often differentiates this from disc herniation.
Lateral recess stenosis with nerve irritation mostly presents without low back pain and rare muscle weakness. The pain may radiate into the ankle and occasionally into toes. Further, radiologic examination often differentiates it from a radiculopathy caused by disc herniation. In the illustration above, the lateral recess stenosis is caused by degenerative changes in the right facet joint, and these are often involved in a back pain condition called facet syndrome.
Multifidus Muscle Dysfunction

The lumbar multifidus muscles are on either side of the spine and play a significant role in lumbar spine function. Dysfunction of this muscle in back disc herniation has a negative affect on function and outcomes following lumbar disc surgery. The degree and presence of multifidus muscle dysfunction can aid in clinical reasoning for a rehabilitation regimen to restore the function of the lumbar spine.
The composition and structure of the muscle in patients with lumbar disc herniation and/or nerve root injury is noted to be a decrease in size and increase of the fat content. By using MRI images, fatty composition of the multifidus muscle at the same level and on the same side as herniation is found to be considerably higher than on the opposite side and has been shown to be a reliable reliable method of assessment
- A 2020 study in the Journal of International Medical Research found both visual grading and quantitative measurement methods of the multifidus muscle demonstrated increased fat infiltration of the muscle on the same side as well as the the same level as the lumbar disc herniation. Additionally this fatty infiltration of the muscle was directly associated with both symptom duration and severity of nerve compression.
In the conclusion, the authors state, “Furthermore, the straightforward and practical visual grading of muscle composition regarding fat infiltration was as useful as quantitative measurement; hence, the present authors suggest that visually grading fatty infiltration of the multifidus muscle may be preferred in daily practice, and should be included in the reporting algorithms.
- A 2020 study in the European Spine Journal demonstrated that fat infiltration of the multifidus with related disc herniation indicates an inflammatory state of the muscle as well as the adipose tissue of the covering around the spinal cord. The inflammation detected was an inflammatory cytokine called tumor necrosis factor (TNF).
- A 2020 study in the journal Spine found the multifidus muscle has a significant role in spinal stability and is associated with fat infiltration and chronic back pain through depleted lumbar stabilization. The authors indicated decrease in fat composition may quantify recovery and the rehabilitation strategies directed muscle activation and lumbar stabilization.
- A 2021 study in BMC Musculoskeletal Disorders indicates herniations at L3/4 and above are referred to as upper lumbar disc herniation, which account for under 10% of lumbar disc herniations. The study shows a correlation between multifidus muscles degeneration and upper lumbar disc herniations. The authors concluded, “Lumbar muscle strengthening training could prevent and improve muscle atrophy and degeneration.”
- Incidentally, a 2021 study in the Spine Journal found that paraspinal muscle fatty degeneration is a predictor of progressive vertebral collapse in osteoporotic vertebral compression fractures, which can lead to spinal deformity and cord compression.
Management Of Back Herniated Disc
Management of a painful disc, spinal stenosis, disc related pain, pain after surgery (post surgery syndrome) is mainly conservative care combining physiotherapy; traction, heat therapy, ice, back brace, electrical stimulation, exercise programs (back pain relief exercises, general back exercises), massage, safe manipulative therapy like Cox Technique, drugs for pain relief and inflammation are often employed. Injections may be recommended and surgery if these above methods fail to provide relief for back pain or resolution.
Below are helpful home methods of conservative management:
Surgery
Microdiscectomy is one of the most common surgical treatments of lumbar disc herniation, with good success rates, however, re-herniation and recurrent low back and/or leg pain can occur in up to 25% of patients. Persistet or recurrent symptoms can result from disc re-herniation, degeneration of the operated segment, or stenosis and the loss of disc height. Re-herniation is a significant problem, with the frequency up to 27% after microdiscectomy.
This technique and variants can lead to disc height deterioration, acceleration of degeneration, reduced axial loading, transfer of load to facet joints, and the recurrence of back and leg pain. Asymmetric discectomy can cause a herniation from the opposite side and aseptic discitis. Limited discectomies done to avoid some of these complications can have a higher rate of recurrence.
- A 2020 study in the International Journal of Spine Surgery indicates the size of the defect in the annulus is a factor for risk of recurrent herniation. A defect of 6 mm or more poses a 27% increase in risk compared to 1% with smaller defects. To preserve the annulus and improve results, a bone anchored annular closure device (ACD) has limited the rate of reherniation and revision surgery.
The authors found that microdiscectomy with ACD, achieved better results, however, factors associated with worse outcomes were: female, higher body mass index, lower initial pain and disability scores, and higher grades of disc degeneration. This shows the importance of annular integrity and the involvement in internal disc disruption.
- A 2020 study in Science Translational Medicine used discectomy with a strategy combining repair of the annulus fibrosus using a photocrosslinked collagen patch and nucleus pulposus augmentation using hyaluronic acid injection. They demonstrated the prevention of degeneration and maintenance of lumbar spine mechanical function.
- A 2019 study in the Journal of Neurosurgery Spine found that with patients suffering leg pain from disc herniation, waiting beyond 6 months for lumbar discectomy is associated with poorer outcomes. Therefore; conservative treatment should be producing results within a 6 month period, indicating the importance of effective therapeutic interventions as early as possible.
- A 2021 study in BMC Musculoskeletal Disorders found that decompressing the nerve via discectomy helped with pain while in motion, however, residual pain after one year was pain during sitting. This was significant for those with Modic changes and disc degeneration. The authors indicated changes in loading of the disc and endplate inflammation may cause residual back pain while sitting.
Smoking And Disc Problems
Most specialists will indicate that nicotine from smoking decreases circulation in small blood vessels and this can have a negative effect on the disc. This makes sense because we know that smoking will decrease microcirculation, and some studies suggest a relationship between smoking and back pain. However, there is another reason that smoking may hurt the disc – coughing. Coughing can cause an increase in pressure on the disc. A cough can produce more pressure on the disc than lifting 25 pounds, therefore; having a smokers cough, a chronic condition from smoking, can actually damage the disc by trauma over a period of time. So, maybe it is a combination of coughing and decreased circulation. We will have to wait for more studies.
- A 2014 study in the Journal of Orthopaedic Research studied vascular effects of drugs on molecular transport of disc and disc diffusion. They were surprised to find that nicotine actually had an effect of increasing blood vessels, however, it did not effect disc diffusion. So, it seems more likely that smoking damages the disc from coughing, rather than decreased circulation. Either way, it is probably a good idea to quit or at least cut down to protect the disc and help disc injuries heal.
Serious Signs Associated With A Back Herniated Disc
The main concern is a cauda equina syndrome, which is a medical emergency requiring surgery. Though rare, cauda equina syndrome is a severe neurologic disorder that can lead to incontinence and even permanent paraplegia if left untreated. The individual nerve roots at the end of the spinal cord provide motor and sensory function to the legs and the bladder. The cauda equina (Latin for “horse’s tail”) refers to the sack of nerve roots with a common covering at the end of the spinal cord that is the continuation of these nerve roots in the low back region.
Cauda equina syndrome most commonly results from a massive disc herniation. Cauda equina syndrome has a range of symptoms, depending on the degree of compression and the nerve roots that are being compressed. Symptoms include severe low back pain, urinary or bowel incontinence, motor weakness or sensory loss in both legs, and saddle anesthesia (unable to feel anything in the body areas that would sit on a saddle). Symptoms may vary in intensity and come on immediately or evolve slowly over time. So, the warning signs include saddle anesthesia, recent onset of bladder dysfunction (such as urinary retention or incontinence), bowel incontinence and motor weakness in the lower extremity. Other conditions that may rarely lead to cauda equina syndrome include osteoporotic vertebral fractures and spinal stenosis.
Summary
A back herniated disc may range from an incidental finding on an MRI with no symptoms, an acute painful condition, to a chronic disabling problem, to a medical emergency. Most herniated discs do not require surgery and will resolve on their own or with conservative care measures. A herniated disc can be classic, with all the typical signs and findings or can be very elusive to diagnose from other conditions. Exciting new therapies like antibiotics, genetics and regenerative medicine associated with herniated discs may help lead the way for more effective therapies in the future.
Considering the importance of the deep lumbar muscles – multifidus, which are small muscles in layers that act to maintain segmental stability, maintain lumbar physiological curve, control facet joint movement, and adjust distribution of vertebral loads and pressures. Decline in function and fat infiltration places one at risk for problems. Here are some exercises to help in prevention and rehabilitation phase of recovery.
- A 2021 study in The International Journal of Psychiatry in Medicine found an association between major depression disorder and chronic lower back pain from disc herniation of the lumbar spine. The authors indicate this problem is associated with higher disability rates, socioeconomic disadvantage, and greater utilization of health care resources. They recommend early detection and combined treatment of depressive symptoms.

 Traction & Inversion
Traction & Inversion Supports & Cushions
Supports & Cushions Belts & Corsets
Belts & Corsets Massage Tools
Massage Tools Relief Supplements
Relief Supplements Topical Relievers
Topical Relievers New Mattresses
New Mattresses Heat Therapy
Heat Therapy Cold Therapy
Cold Therapy TENS Therapy
TENS Therapy Posture Braces
Posture Braces Ergonomic Aids
Ergonomic Aids