Spinal Injections For Relief Of Neck & Back Pain
An alternative to surgery and when symptoms of spinal problems continue despite attempts at therapy, spinal injections may be considered.
Pain management specialists (anesthesiologists, physiatrists, radiologists) are performing these injections with increasing frequency. When neck and back pain symptoms persist, they can interfere with daily activities of life as well as the capacity to do certain therapy activities like rehabilitation exercises. The symptoms can be localized pain in the neck and back along with pain, numbness or weakness of the arms and legs. In these cases, injections may offer relief of pain and provide a means to offer rehabilitation with strengthening and stretching. While there are no guarantees and injections are not without risks and controversy, they offer an option prior to consideration of surgery.
Types
Epidurals:
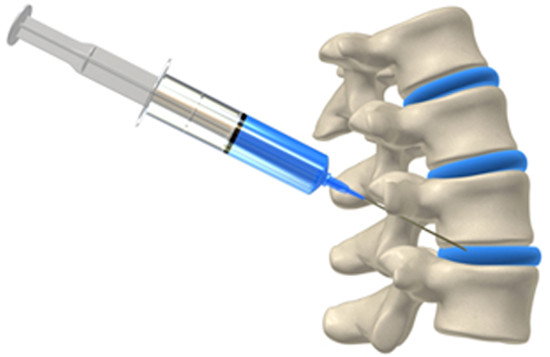
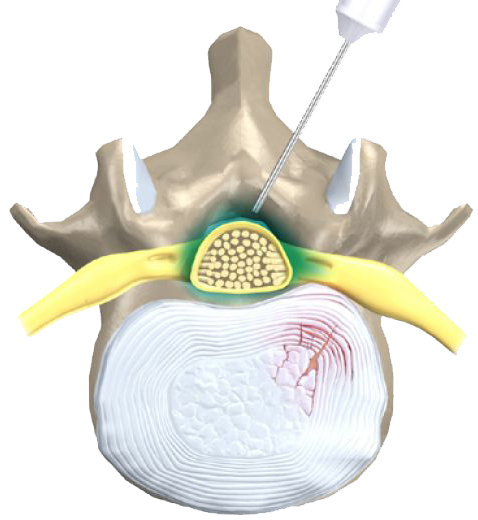
Steroids to reduce inflammation can be injected into the space around the covering of the spinal cord called the dura. The nerves that exit from the spinal cord can be surrounded with the anti-inflammatory steroid. Epidural injections are done to alleviate pain radiating into the arms and legs from a pinched spinal nerve or disc herniation.
The types of injections, such as interlaminar or transforaminal refer to specific locations in the spine to effect areas where the problem is stemming from and depends on the diagnosis. Spinal injections may be done under the guidance of imaging to increase accuracy. Epidural injections may use steroids, an anesthetic or combination to reduce inflammation and alleviate pain. These injections are therapeutic.
The injections may be diagnostic, often involving only anesthetic to help determine if a specific area or nerve is the cause of pain. Relief of pain confirms the location as the cause of pain, while lack of response leads to further investigation. Recent literature indicates epidural injection may not be effective for relief of spinal pain related to Modic degenerative changes.
Facet Joint Injections
Facets joints are located in the back of the spine and provide gliding motion. These joints can become injured or inflamed due to arthritis. Facet joint pain can be local back or neck pain, but they can also cause pain that runs into the extremities that mimic disc problems. Facet joint spinal injections can be used to alleviate this pain or to help in diagnosing if the problem is related to the facet joints.
So, facet joint injections can be therapeutic or diagnostic. If the facet joints are determined to be the source of pain, procedures that block or permanently destroy the small nerve supply to the joints can provide a solution to this problem. These procedures are similar to spine injections, except there is a probe that is inserted to destroy the nerves.
Nerve Root Blocks
These are often called selective nerve root blocks. They target specific nerves to inject the anesthetic and/or steroid anti-inflammatory medications. This is similar to an epidural, but seeks to locate specific nerves for therapeutic or diagnostic procedures. These are used under guidance of imaging like ultrasound (not the same as therapeutic ultrasound) or fluoroscopy and contrast may be used.
Sacroiliac Joint Injections
Sacroiliac injections are administered like facet joint injections only into the pelvis area. The sacroiliac joint can be responsible for back and leg pain. Injections under x-ray guidance will administer an anesthetic and this should decrease the pain if the sacroiliac joint is involved. Steroids may also be injected, therefore we see that they can be both diagnostic and therapeutic and this is often why a combination of an anti-inflammatory agent like a steroid and anesthetic are used.
Other Injections
There are other types of injections like intradiscal injections, where the injection is delivered inside the disc. There are also studies ongoing that are using different medications or agents for spinal injections that are promising for conditions like disc degeneration.
- A 2020 study in the Global Spine Journal did an analysis of 4 randomized controlled studies which showed no outcome difference between therapeutic agents (growth factor, fibrin sealant, or stem cells) and control saline injections into the disc. All groups reported decreased pain and disability scores, therefore future studies are needed to indicate therapeutic benefit of any injection into the disc regarding agent used.
Are They Safe?
They generally are safe procedures, and any complications are most often mild and short lasting. Typical effects from steroids can be flushing of the face, appetite increase, irregularity of menstrual cycle, increase in blood sugar, diarrhea and nausea. Rarely, spinal injections can cause more serious side effects, like increased pain, spinal headaches, weakness of muscles, infection, bleeding, nerve injury, paralysis and others.
- A 2013 edition of the journal Surgical Neurology International performed a review indicating spinal injections pose serious side effects, major risks and complications and provide no long term results. They indicate insurance companies are promoting increased payments for injections performed without the benefit of guided imaging. The study notes the risks of steroid injections in the spine indicating that injections, specifically epidural and transforaminal steroid injections, are not safe and effective.
Although commonly performed, many without complications, this article sheds some light of the risks and complications. The article notes lack of FDA approval and rather disturbing statistics from the CDC. Those who are somewhat technically oriented and/or prone to researching procedures prior to having them done may read this rather comprehensive article and discuss any concerns with their doctor.
I would insist that ANY injection be done GUIDED and with an experienced Doctor, in a suitable setting.
If you have any allergies to steroids, anesthetics or contrast agents, diabetes or high blood pressure that is not under control, bleeding disorders or coagulation problems or skin infection where the injection would be administered, you would not be a good candidate for a spinal injection.
- In a 2018 edition of Surgical Neurology International outlines risks and complications of cervical epidural steroid injections in an updated review. It is always worth considering the source, however, this does not nullify the findings.
The authors indicate that injections may done with little or no indication for medical necessity versus risk. Additionally, “Furthermore, these injections are increasingly required by insurance carriers prior to granting permission for definitive surgery, thus significantly delaying in some cases necessary operative intervention, while also subjecting patients at the hands of the insurance companies, to the additional hazards of these procedures”.
We all want to avoid surgery, however, when there are clear indications, avoiding for either or both psychological and financial reasons may promote unnecessary interventions that may foster long term chronic pain and complications.
- In a 2019 edition of Surgical Neurology International which concludes, “The present case report is an example of long-term pain management with multiple medications, including opioid use and performing interventional pain procedures, while avoiding early surgical correction of cervical disc herniation. This resulted in years of suffering with pain and serious morbidity from opioid overdosing. Surgical intervention was definitive in terms of ultimately improving her pain and reducing her reliance on opioid analgesics.”
The best decisions are made by the best doctors with the best intentions. Financial gain and plays on fear are not good intentions. The increasing complexity between the two, which often involves different entities with sometimes opposing intentions, is not good for the patient.
Imaging Prior To Spinal Injections
- MRI imaging prior to injections is advisable. A 2019 study in The Spine Journal indicates that MRI findings 43% of injections were changed from the initial decision. 36% revealed a different level affected, 22% revealed a facet joint pathology, and in 16%, a different nerve root was affected.
It is evident that there is utility in obtaining proper imaging prior to the procedure, and that it does reasonably impact results on injection planning. The authors of the study concluded, “In clinical practice, MRI prior to injection frequently changes management decisions in the planning and delivery of lumbar spine injections.”
Precision is important to results in any specific application. Imaging to identify the pathological generator of the symptoms and guided application to insure that pathological generator is specifically targeted is key to achieving the best results. The study was done specifically on epidural steroid injections (ESI), however, it is reasonable to assume this clinical reasoning would also apply to anesthetic or mixed applications as well.
Response To Spinal Injections
Responses to injections are generally well. An indication that they may not work well is when there is a complaint of both back and neck pain, and symptoms that recur more than a year after a previous injection. The measurements of success often involve different measurement outcomes.
- A 2019 study in the journal PLoS One indicates that instead of outcome assessment measures, including visual pain diagram measures, that residual symptom percentage (percentage of improvement indicated) is the most practical in representing patients’ improvements after spine injections.
