Facet Joint Syndrome Complicates Neck And Back Pain
The facets are parts of the bones in the neck and back which form joints that guide motion. Facet joint syndrome pain, also known as facet syndrome is common among patients with chronic back and neck pain. In the neck, injuries to the facet joints are a common cause of pain after whiplash and is a major source of clinical importance.
 As you can see from this graphic, the facet joints produce pain when arching back. Irritated facets approximate and cause inflammation. This limits backward motion of the neck and back and the typical posture of those in pain is one of being bent forward to move the joints away from each other.
As you can see from this graphic, the facet joints produce pain when arching back. Irritated facets approximate and cause inflammation. This limits backward motion of the neck and back and the typical posture of those in pain is one of being bent forward to move the joints away from each other.
Facet joints are implicated as a major source of neck and lower back pain. Both neck and back facet syndromes have been described in the medical literature and biomechanical studies have shown that these facet joint capsules undergo significant strain during spinal loading (lifting or sitting), especially when they have degenerated.
- Studies have demonstrated pain sensitive nerve endings in facet joints mechanically sensitive receptors which become activated with inflammation. A 2015 study in the journal Osteoarthritis and Cartilage indicates facet joint degenerated tissues contain inflammatory chemicals, ingrowth of blood vessels and chemicals that activate pain nerve fibers. These factors cause pain and progression of the facet syndrome condition, similar to the process involved with disc degeneration.
Biomechanical studies indicate that rear end motor vehicle impacts give rise to excessive deformation of the capsules of facet joints, often a cause for persistent pain after whiplash trauma, and injury to the facets in the lower back may be produced by lifting and twisting to one side.
 Facet syndrome is often associated with chronic pain. Illustrated here is the degenerative process often associated with arthritis. The front part of the bone with the disc is usually the first to begin this process of degeneration. Soon after, the decreased height of the bones places undue stress on the facet joints which start to degenerate. This causes additional inflammation and allows a smaller window for pain free motion. This can often result in facet syndrome pain.
Facet syndrome is often associated with chronic pain. Illustrated here is the degenerative process often associated with arthritis. The front part of the bone with the disc is usually the first to begin this process of degeneration. Soon after, the decreased height of the bones places undue stress on the facet joints which start to degenerate. This causes additional inflammation and allows a smaller window for pain free motion. This can often result in facet syndrome pain.
- A 2021 study in the International Journal of Spine Surgery found that pre-existing facet degeneration is correlated with long term symptoms after whiplash. The authors propose facet joint instability due to joint capsule rupture as a potential mechanism for non-recovery.
There are many reasons for this degenerative process, often associated with arthritis. Many have wrongly suggested that this process is normal with aging. It is normal for degeneration to occur with aging, however, it is not associated with pain. Degenerative disc disease is painful and often disabling. Radiographic signs of significant decreases in disc space are most often associated with pain and the disease process, not normal aging! Genetics have been found to be of major importance in addition to loading history (heavy lifting or prolonged sitting). Unfortunately, with facet syndrome in the lower back, typical back supports that accentuate the lumbar spine lordosis used in seats may be of no help and may even aggravate the condition.
In the lower back, facet syndrome is characterized by: low back pain; pressure soreness at the level of the facet joints involved; leg pain, but not following a radicular pattern of a pinched nerve; pain increase during rotation movements; greater pain during extension with respect to flexion; pain in the transition from the seated position to the standing one; reduced range of movement with greater stiffness in the morning.
- According to a 2018 review report in Insights into Imaging this is a common source of back pain and facet joints has been estimated to account for 15 to 45% of low back pain, with pain originating in the synovial membrane, cartilage, bone, or fibrous capsule of the facet joint.

Notice the neck is much more specific in referred pain than the lower back. The lower back may have complications that refer pain in a wide range. It is possible to have more pain in the referred area than the back as I relate to my experience below.
- A 2020 study in the European Spine Journal evaluated over 200 patients using kinematic magnetic resonance imaging and found that facet osteoarthritis grades were correlated with disc degeneration at the L5/S1 level. This indicates the facet joint space width decreases significantly with increasing grade of disc degeneration.
If the back pain exercises do not help or make pain worse, then you may have facet joint syndrome problems and must avoid extension and rotation – usually to one side. Your problem may be degeneration and chronic or long standing back pain or it may be from an injury to the facet joints usually from lifting and twisting to one side. This recently happened to me as I was lifting a vacuum cleaner. I jammed the facet joints on the right side and immediately experienced pain.
The pain radiating from the back, around the buttock and into the groin was quite disturbing. I have severe degeneration of the L5-S1 disc and, as a consequence, have developed degeneration of the lumbar facets. I first noticed the facets were becoming a problem when using a back support that extends the lower back region which increased the pain. One of best solutions I have found for seating support is an active seating cushion, which also helps with reducing spasm of the Quadratus Lumborum muscle when seated for long periods, especially when driving.
With facet joint syndrome, you should do back exercises (1, 2, 3, 6, 7, and 9). Additionally, specific chiropractic adjustments can help. The adjustments must be done on the correct side. In my case, a right L5-S1 facet compression injury, I used a Medrol Dose Pack to reduce inflammation, hot packs, massage and while I was backing into a parking space, I twisted to the right with my right arm around the back of the car seat and kept my torso straight at which point a loud release of the joints were noted and the pain subsided for the first time. I do not suggest you try this, a chiropractor would test the joints and perform a right side posture lumbar adjustment to the same effect. A bit painful, but effective. A concentrated massage along the pain referral areas and topical applications to the affected areas finally got rid of the pain.
Another area of concern is lifting injuries and the discussion regarding while lifting, you must retain the normal curve or arch in the back under back posture. When you have damage to the facet joints resulting in a pain syndrome, you should not arch your lower back when lifting. It is also important to use a stool when standing for long periods as when using an ironing board and to flatten the lower back when raising your arms above your head. Pain in the lower back that is relieved by sitting is a sign of lumbar facet joint syndrome.

Pain patterns are a clue and there is much overlapping, but it helps in trying to determine the difference between disc pain and facet joint pain – there can be both!
- A 2020 study in Neurospine examined the cervical spine for facet joint degeneration and found it was related only to Modic changes and uncovertebral joint degeneration (joints only in the cervical spine). Indicating that in the neck, degeneration of the facet joints can occur more independently than the lumbar spine.
- A 2024 study in World Neurosurgery found aging, poor cervical alignment, low bone mineral density, disc degeneration, and modic changes posed a higher risk for cervical facet joint degeneration.
The facet joints are a crucial anatomic stabilizer because they play an important role in load transmission, in flexion and extension while restricting rotation. Together with the disc, the facet joints transfer loads and guide and constrain motions in the spine. This ensures the normal health and function of the spine during loading, but damage to ligaments (capsular around the joint) can lead to joint dysfunction and degeneration, which disrupt facet responses

Where there is damage to the ligaments or from slow stretch over a long period as in poor posture, directing treatment at the ligament in order to regenerate and tighten the ligament can help. This is a part of regenerative medicine known as prolotherapy.
- A 2021 Case Reports Radiolology noted a 41 year old male presented after a fall with neck pain and the initial imaging missed a “subtle abnormality” (C5/6 subluxation). This is typically what many Chiropractors specifically look for and treat. The patient later presented with with neck pain subsequent imaging demonstrated a bilateral facet dislocation with severe deformity which required spinal fixation surgery.
If all else fails, the medical community has facet joint injections and nerve disruption techniques that you may wish to consult with. A surgical procedure called radiofrequency rhizotomy might be necessary to relieve pain and improve mobility. Radiofrequency rhizotomy, also called radiofrequency neurotomy, is the surgical “de-nerving” of the facet joint.
Facet Joint Injections
When home measures or conservative care like chiropractic, physical therapy and medications fail to provide satisfactory relief, injections can be a good alternative prior to considering surgery. Injections for facet joint pain can serve 3 purposes: 1) For pain relief. 2) As a diagnostic tool. 3) Both.
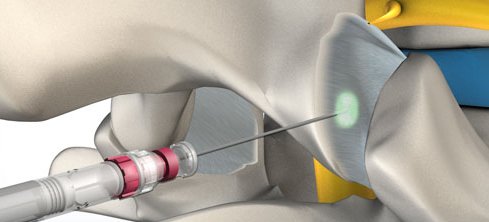
By injecting either a analgesic like lidocaine, an anti-inflammatory like cortisone, or both, relief of pain can indicate that the diagnosis of facet joint pain is valid. This may be done with an anesthetic to “block” the nerve, confirming the source of pain. By including an anti-inflammatory, longer term pain relief can be the objective.
Getting a facet joint injection is a minimally invasive procedure, usually lasting about 15 minutes. Lying down on a table, the skin over the joint is numbed and a needle is guided into the joint using a type of live x-ray called fluoroscopy. With this procedure, a contrast dye is used to confirm exactly where the medications will go. The injection slowly releases the medications.
The results can provide immediate relief from the anesthetic, and longer lasting relief in a couple of days or perhaps a week from the anti-inflammatory. Results may be about 50%. With no relief of pain after a week, additional testing may be done to determine if a nerve that supplies pain sensations (medial branch) would respond to similar injection. With pain relief on injection of the medial branch nerve, further consideration for radiofrequency neurotomy/ablation, which is a type of injection using a radiofrequency energy heat probe to destroy the nerve function.
- A 2022 study in World Neurosurgery found benefit with SPECT-CT guided facet injections after failed prior facet injections. SPECT-CT is Single photon emission computed tomography and is able to provide true 3-D information.
- A 2014 study in the Pain Physician Journal observed 55 patients who underwent cervical radiofrequency neurotomy for chronic whiplash symptoms. There were improvements in disability, pain and psychological distress 3 months following the procedure. The lateral branch nerve is the focus of pain from the sacroiliac joint.

Injections for facet joint syndrome may be repeated a few times a year if necessary. The neurotomy may provide relief for up to a year or more. Typically, the relief may be shorter and the nerve usually regenerates. Success is better for the neck than the lower back, however some will not respond at all.
I have always suggested that spinal injections should be done guided (using appropriate assisting imaging), instead of “blind”. It has always been my assumption that a more precise location leads to better results instead of basing technique on expediency or cost incentives. I think this is common sense and I have seen some rather poor or adverse outcomes with blind injections.
- A 2019 study in the Journal of Back & Musculoskeletal Rehabilitation assessed the efficacy of guided versus blind injections for facet syndrome. The results indicated ultrasound guided injections produced better results for pain and disability at the 6 week evaluation, than those receiving blind or non-guided injections.
I developed facet syndrome of the lower back which referred pain to the hip. It was so bad I had to limp when walking and could only sleep on my right side. In fact, the only symptom was hip pain, which the orthopedist diagnosed as a torn labrum of the hip and referred for MRI. This would mean surgery. The MRI appt was in 3 months and I could no longer bear the pain, so I went to my pain specialist.
He noticed how I was sitting and said it was not a torn labrum, and after a quick exam diagnosed facet syndrome. I had two injections that provided some relief, but pointed to the right direction. He changed the MRI to the back instead of the hip. After confirmation, he performed a neurotomy, which provided good relief. With some residual pain, 3 months later, a second one was performed and it has been very successful.

- In fact, a 2020 study in the Journal of Orthopaedic Surgery & Research found that radiofrequency neurotomy/ablation mentioned above, under new endoscopic guidance (ERFA) for chronic low back pain from facet joint arthritis may achieve more accurate and definite result, leading to longer lasting pain relief.
- Confirming this, a 2020 study in Clinical Neurology & Neurosurgery used Endoscopic Facet Joint Denervation (EFJD) for chronic lower back pain and concluded it is a promising technique with the advantage of direct visualization of the facet joint and the nerve, allowing for more accurate denervation. They found it contributes to significant and sustaining pain reduction and improvements in subjective quality of life.
- A 2020 study in Annals of Palliative Medicine found that destruction of the posteromedial ramus of the spinal nerve significantly improved low back pain, improved function and enhanced quality of life at 12 week follow-up.
- A 2020 study in Therapeutic Advances in Musculoskeletal Disease found endoscopic denervation, which guarantees a more precise approach to anatomical structure, provides significant analgesia at 2 year follow up for low back pain.
- A 2021 study in the journal Spine found there were no difference between injections and radiofrequency denervation of the cervical facet joints at 6 months follow-up, however, there was a difference in the long-term effect after 6 months follow-up in favor of the radiofrequency denervation treatment.
- A 2019 study in the journal Medicine (Baltimore) used amniotic membrane and umbilical cord particulate injections for neck pain patients with confirmed facet injury or facet joint arthritis. Patients received a single intra-articular injection. At 6 months follow-up, pain was decreased and all patients stopped prescription pain medications, including opioids. No adverse events, repeat procedures, or complications were reported. This is a move towards regenerative medicine.
- A 2022 study in The Spine Journal found injections were much less effective when active endplate changes were found, a condition called Modic changes.
Facet Syndrome: Adverse Reactions To Injections
- According to a 2014 study in Pain Physician Journal, the adverse reactions are minimal. Vasovagal reaction occurred as the most common immediate adverse reaction and injection site soreness was the most common delayed reaction. Vasovagal reaction can be a number of things: dizziness, lightheadedness, weakness, nausea, palpitations, blurred vision, feeling cold or warm, sweating and possibly fainting.
More serious events are rare
There are some very rare but potential complications. Those on medications for blood thinning, have an infection or are allergic to any medications or contrast agent used should not have facet injections. Consult with your doctor regarding any potential complications from infection, nerve or spinal cord damage from the needle, bleeding or artery damage from injections for facet joint syndrome.
Facet Tropism
Another problem that can be found with the joints in the spine is asymmetrical facet joints. This means the joint has a different orientation one one side than the other. This condition can effect the motion of the joints, which is to glide smoothly.
 Like train tracks, they need to be parallel for the train to glide smoothly down the tracks. If you have a section of track on one side that is oriented differently, disaster could result. While it is most likely a congenital situation – from birth, and may not cause pain, in more severe cases, or where there is degeneration, this can cause a facet syndrome type of pain.
Like train tracks, they need to be parallel for the train to glide smoothly down the tracks. If you have a section of track on one side that is oriented differently, disaster could result. While it is most likely a congenital situation – from birth, and may not cause pain, in more severe cases, or where there is degeneration, this can cause a facet syndrome type of pain.
- A 2017 study in BMC Musculoskeletal Disorders found tropism in the cervical spine was most common at the C2/3 level, the upper cervical spine, and was associated with facet joint degeneration.
- A 2017 study in the Spine Journal found that facet tropism at the C5/6 level increased disc pressure as well as facet joint contact force and may be a risk factor for disc degeneration and/or facet joint syndrome degeneration.
- A 2017 study in BMC Musculoskeletal Disorders found a significant correlation between lumbar facet tropism and degenerative conditions, including lumbar disc herniation at the L4/5 and L5/S1 levels.
- A 2018 study in International Surgery concluded, “Facet asymmetry is significantly associated with lumbar disc herniation at the L4 to L5 and the L5 to S1 levels, whereas there is an obvious association with the side type of lumbar disc herniation at the L5 to S1 level.”
- A 2019 study in Clinical Neurolology & Neurosurgery found that facet tropism at the L5/S1 level are more likely to develop lumbar spinal stenosis (narrowing of the spinal canal) due to hypertrophy of spinal ligament called the ligamentum flavum.
- A 2023 study in The Spine Journal confirmed that facet joint tropism, high pelvic incidence (excessive lumbar lordosis or sway back) and low intervertebral height index were significantly associated with osteoarthritis of the facet joints at L4-5. This plays a significant role in the development of lumbar spinal stenosis.
- A 2021 study in Acta of Bioengineering and Biomechanics indicates facet joint tropism, which is angular asymmetry between the left and right facet joint orientation is a developmental abnormality that can cause stress and pain. Severe tropism causes more significant changes in disc bulging on the side of the altered orientation of the joint. This increases stress on the joint 10 times compared to the physiological normal orientation. Disc degeneration and herniation may result over time.
Tropism needs to be considered as it poses biomechanical factors that effect treatment parameters. Most commonly seen at the L4/5 level, the extra stress is seen in all motions, however, the annular fibers of the disc are particularly sensitive to rotational forces. Often overlooked or considered as a normal variant, it can lead to failed treatments and chronic pain.
- A 2019 study in Skeletal Radiology found that patients with radicular pain from a herniated lumbar disc were less responsive to treatment with transforaminal epidural steroid injections. The response was about 50% less for patients with tropism, therefore, the authors of the study suggest facet tropism should be included in a discussion regarding the benefits of the procedure.
Synovial Cysts
The facet joints have a membrane around the articulation filled with fluid. Associated with degenerative changes, however, usually rare, a cyst may form in the joint that may cause pain or may grow to an extent or herniate, that it causes radiculopathy or pinches on a nerve.
- A 2019 study in the journal World Neurosurgery found these cysts may be associated with an unstable spinal segment. The authors found about 89% were associated with facet joint syndrome or degeneration. Most are found in the lumbar spine at the L4/5 level, which is the most mobile lumbar segment; however, they do occur in the cervical spine.
They may be asymptomatic, however, can cause a great deal of pain and even cause spinal cord compression in severe cases. Because there is a high rate of recurrence with resection or aspiration, surgical facetectomy (removal of the facet joint) and fusion is usually the most effective method.

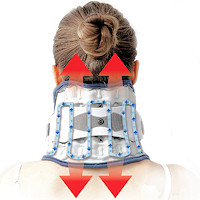 Neck Traction Devices
Neck Traction Devices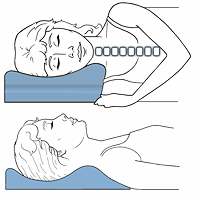 Cervical Pillows
Cervical Pillows Neck Support Collars
Neck Support Collars Muscle Therapy Tools
Muscle Therapy Tools Head Supports
Head Supports Topical Pain Relievers
Topical Pain Relievers Traction & Inversion
Traction & Inversion Supports & Cushions
Supports & Cushions Belts & Corsets
Belts & Corsets Ergonomic Aids
Ergonomic Aids New Mattresses
New Mattresses Relief Supplements
Relief Supplements