Antibiotics For Back Pain
 We have discussed previously about back pain and antibiotics. We have also looked at Modic changes and back pain, where you can even use an online form to get an idea if you might be suffering from this. This is a continuation to answer some frequently asked questions. You should be familiar with the previous material, which gives a good overview. I will answer some of the more frequently asked questions regarding, but first, I need to clear some things up a bit.
We have discussed previously about back pain and antibiotics. We have also looked at Modic changes and back pain, where you can even use an online form to get an idea if you might be suffering from this. This is a continuation to answer some frequently asked questions. You should be familiar with the previous material, which gives a good overview. I will answer some of the more frequently asked questions regarding, but first, I need to clear some things up a bit.
We will use the term “antibiotics for back pain”, however, this is not a proper way to describe it. Antibiotics are not for back pain! Antibiotics are for the treatment of specifically Modic Type 1 Changes in the lower back that result in chronic back pain and are related to infection. So, if you do not have Modic type 1 changes on MRI and typical signs that they are the cause of the pain, it does not matter if you have back pain, antibiotics should not be used.
Why Antibiotics Are Used For Back Pain
Modic type 1 changes are findings on MRI that indicate a rapidly progressing and deforming type of degeneration and inflammatory condition in the spine. Previously thought to be just a finding or perhaps an indication of forming bony outgrowths called osteophytes, research has clearly shown Modic changes to be specifically related to back pain. Some research indicates over 40% of individuals suffering from chronic, non-specific back pain will have Modic changes, with 6% of general populations displaying Modic changes.
When there is a break in the disc which allows communication to the outside as seen with some disc herniations, normally harmless bacteria found in the mouth and skin may find a home within the disc space. As the bacteria thrive in this poorly oxygenated environment, they secrete a substance which dissolves bone. This substance gets into a spinal bone through a break in the endplate, which is normally a secure barrier between the disc and the bone. The bacteria do not come outside of the disc and attack the bone from the outside.
Now, bone is not a solid block. It has a scaffolding structure inside and there is bone marrow. The bacteria secrete this substance called propionic acid which causes breaks in the scaffolding. The structure is weak and it does not take much to cause a break called a microfracture. From the inflammation, chemicals are released that cause an ingrowth of nerves, which are especially sensitive because they lack the normal protective covering.

In this illustration, you can see the normal structure of a spinal bone (A). Notice the structure of the scaffolding. In (B) the scaffolding has been destroyed and the red bone marrow is attacked. (C) Shows a closeup of a break, notice a nice structure on the right and a rather ominous looking break to the left. The break is pointed and (D), there are very sensitive nerves which can be irritated in this process.
A 2021 study in Pain Medicine found 3 categories of nerves are found the disc: sensory nerves, perivascular nerves, and mechanoreceptors. These are capable of producing pain. While nerves were consistently found within the outer layers of the annulus fibrosus. Ingrowth of nerves into the inner annulus fibrosus and nucleus pulposus was found only in degenerative and disease states.
What does this feel like?
A microfracture is a sharp pain in the back that may take your breath away. It can happen when you lift, however, because the structure is so weak, it can happen when turning over in bed. Typically, there is a history of back pain that comes and goes, like a cold. The pain becomes chronic and is worse in the morning, eases up during the day and gets worse in the evening. Usually, there have been many attempts to alleviate the pain; medication, physical therapy, massage, chiropractic and other forms of treatments which do not provide anything other than short term relief.
While many standards of care indicate exercises for low back pain and it is frequently prescribed, exercise in those suffering chronic back pain from Modic 1 changes are made worse with exercise. Let me repeat that – The Condition Is Made Worse With Exercise! The most prominent feature is pain on bending forward (lumbosacral flexion). You learn to bend with your knees, but any kind of forward bending with your back is painful and feels like you have no strength in this position. There can be radiating pain into the leg. It is back pain that is always there. It may be more or less, but it is always there. Experiencing microfractures is scary pain! The pain limits your ability to manage normal activities and you may be disabled. In other words, it has a huge impact on your life.
Those with this condition are often treated like it is all in their heads. Ever feel like this? You have been trying everything, but nothing works and finally you are given medications for depression. It is true that chronic pain can effect the brain. Hypercentralization is a term used for this and it is real. Think of a phantom limb; a limb is lost, but the person may still feel pain or the sensation that it is still there. So, you take the medication, and it may help you deal with the pain, but the pain is still there. You concede that this is how it will be and hope you will not need surgery in the future. Chances are you may, as this is an unstable condition in the lower back and procedures like fusion surgery can help.
Now imagine, you finally are told there is a pain generator; an actual possible physical reason for your pain has been located. How would you feel? Hopeful? Is taking antibiotics the answer?
What Are My Chances For Getting Better Taking Antibiotics For Back Pain?
If you have been properly evaluated and it is determined you have; MRI verifiable Modic 1 changes with absence of claw signaling on Diffusion Weighted MRI, a history that matches the profile of those that suffer from this condition as described above, positive signs on physical examination, have no allergies to antibiotics, are not pregnant or nursing, have no liver or kidney problems, do not experience negative side effects to antibiotics like severe rashes, stomach upset or diarrhea, you will have about an 80% chance taking the double dose. That is if you can handle almost 4,000 mg of Amoxicillin Clavulanate a day for 100 days! Then, waiting up to one year for results! So, taking antibiotics is not to be taken lightly and should be done only under the supervision of a practitioner who is certified in Modic Antibiotic Spinal Therapy for best results. While there is no longer certification, you can contact us and we will try to help.
In Europe, taking antibiotics for back pain is more accepted and widely used. Despite this, there is still a high prevalence of patients that are uninformed regarding the process and how to get the best results, presumably from a lack of education. This indicates many doctors are prescribing antibiotics without employing the services of a certified MAST practitioner. I have presented a lot of information here, and it is my hope that individuals undergoing antibiotic therapy for back pain related to Modic type 1 changes will achieve better results by simply reading this information and make myself available, at no charge, for consultation.
What Does Getting Better Mean?
Once the bacteria are killed and the bone has a chance to heal – up to 1 year, you may get a range of relief. Many individuals have had chronic pain for a long time; there may be significant levels of degeneration, muscle, ligament, nerve or joint damage and the foundation is less than normal. Therefore, you may experience different levels of getting better. If you have been suffering for years, how much relief would you be satisfied with in a year from now? 50%?, 75%? 25%? These are all ranges and your back pain may not be due strictly to Modic changes. Basically, many people would be satisfied to be able to do laundry again, or ride a bike for a half mile instead of just around the block.
Would you be satisfied with a 50% reduction in pain and increase in ability? Might this mean you can go back to work, get a good night’s sleep or play with your children or grandchildren? For some, being able to just bend over and kiss their child goodnight in bed without being in agony or having to assume an awkward posture would be healing. For some, it is a complete return to normal and ability. So, getting better is relative and taking antibiotics for back pain is not a magical cure. Set reasonable goals when first starting your antibiotics for back pain.
Can I Maintain Normal Activities?
No! You must reduce stress on the spine during the 100 days. While you do not have to lie in bed all day, you must take it easy. Remember, exercise makes this condition worse. Why? There is basically a fracture and a boil. The boil is from the inflammation inside the bone, which forms a liquid like a boil, and we have discussed the microfractures and sensitive nerves. So, if you had a boil and a fracture in your wrist, would you lift weights? Do push-ups? That is why a certified Modic antibiotic spinal therapist knows the value of having a spouse or significant other present during the initial 45 minute to one hour education session. You would not just give a diabetic insulin and a needle and say, “good luck!” It is important to have a spouse present so they do not have to come home and say, “they said you will have to do the chores now”.
You will have to learn how to pace yourself. If you walk a half mile and the pain is worse after, later on or the next day, you must go back to the quarter mile, if that does not make it worse. It is important not to get the area inflamed or get more microfractures from lifting or overdoing it. Before taking antibiotics, you might have said, “I know this will make it worse, but I have to”. Now, you must not, get some help, as difficult as it might be to ask or say that you can’t. Your outcome depends on it and you may only get one chance at this. You will be able to do more when the bone is healed, there are no more microfractures and the nerve fibers are gone.
Starting to get the idea that taking antibiotics for back pain is not as easy and simple as it sounds?
Can I get Modic Changes In The Neck?
Many individuals with Modic changes in the back also have neck pain. Modic changes can occur in the neck, however, it is observed about 5 times less frequently than in the back. So, will antibiotics for back pain also work for neck pain? Well, the theory is the same, however, there are no studies in this area, therefore, the answer right now is, I don’t know. It is possible, but more studies and research are needed. There are no studies currently that indicate taking antibiotics for neck pain will produce results similar to those seen for back pain…. not yet!
My Antibiotics Are Finished And I Still Have Back Pain?
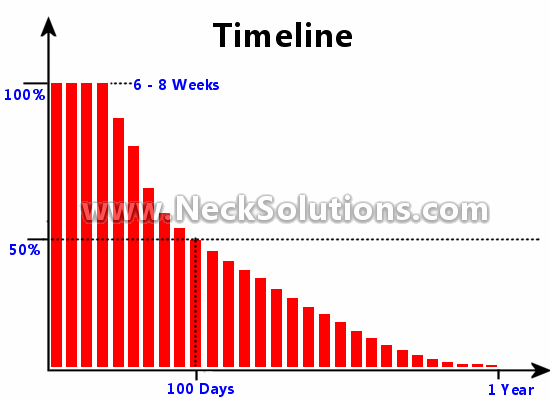
While we have discussed this before, it deserves reviewing it again. After the 100 days, the treatment is only half done. One thing that is important to do is to print out this graph or, if you have been given one by a certified Modic antibiotic spinal therapist, put it on your refrigerator. Make a copy and also place it in other areas where it can be easily seen. This will give you a bigger picture of where you are and how the healing progresses related to time. After you are finished the antibiotics, you are half way through the healing period. You must remember that changes occur gradually over time and you may not notice these changes as they happen. Bone healing is slow. Remember your original goals and how far you have come. Can you empty the washing machine? Can you ride your bike a half mile? Many times we will forget how bad we were.
Do I Really Need To Take Antibiotics For Back Pain? Can I Fix It On My Own?
Remember, antibiotics are not for back pain; they are for infection related Modic type 1 changes visible on MRI imaging, along with a history and physical findings typically found with this condition. That said, you can fix this on your own without taking antibiotics for back pain – just let it heal! OK, this will take from 10 to 12 years and you must hope that the brain has not become sensitized by the pain.
Take pneumonia for example; in the past, if you got pneumonia, you would stay in bed and eat soup for 3 months, provided you had someone to help you. There was a very long recovery period. Some of them died. Then antibiotics came along and you would take them and in a week or two, you were well on your way to recovery. Similarly with taking antibiotics, you will take them for 100 days and recovery takes 6 months to a year. If not, 10 – 12 years! But wait, Modic 1 changes often progress to Modic 2 and then to Modic 3 and, Modic 2 or 3 changes have been noted to change back to Modic type 1! The picture gets a little complicated. Nevertheless, taking antibiotics may provide a cure and end this possible long term cycle of disease.
Why Do I Have Modic Changes When I Never Had Leg Pain, Which Is Normal With A Disc Herniation?
Modic changes are associated with disc herniations, however, even though leg pain is commonly experienced with a disc herniation, leg pain or typical sciatica is only experienced with direct nerve pressure. If the herniation is away from the nerve and there is not much inflammation, you may experience no leg pain at all, and you may not notice much back pain either.
Once I Am Better, Will It Come Back?
Only if you get another disc herniation, because this is the point where the bacteria can enter the disc, thrive and produce acid which dissolves the inside of the bone. This is not very likely.
Why Do I Have To Take Such Large Amounts Of Antibiotics And For Such A Long Time?
Because there is no vascular system in the disc, it is difficult for the antibiotics to get into the disc and it takes a long time before enough amounts of the antibiotic are able to kill all the bacteria.
Are There Any Treatment Options For Back Pain Related Modic Changes?
Yes, there are other treatments that have been used with some success. In a September 2011 issue of the Arthritis & Rheumatism journal, there was a report of a 31 year old man with Modic 1 changes, who received a intradiscal corticosteroid injection – injection of steroids into the disc. The report indicates rapid relief of pain and no Modic changes indicated 1 month later on MRI. Now, this is not a large study, just one individual. I have not seen any follow up from the individual report, however, this does emphasize the inflammatory nature of Modic 1 changes. A February 2011 article in the Spine Journal studied a number of individuals with different types of Modic changes, not just type 1, and indicated steroid injections may be a short term effective treatment for those who had Modic changes and refused to undergo surgery after failed conservative treatment. Other studies have also shown benefit for intradiscal injections and Modic changes.
A March 2014 issue of the BMC Musculoskeletal Disorders journal studied the effects of zoledronic acid injections on various types of Modic changes, again, not just Modic type 1 changes, noting positive results. It was indicated that zoledronic acid effectively reduced low back pain intensity in the short term, while reducing NSAID (like Ibuprofen) use for up to 1 year. Zoledronic acid is a bisphosphonate drug. In the study, 95% of those injected experienced fever, flu like symptoms and joint pain (arthralgia). It is used to treat osteoporosis and to prevent fractures in cancer patients. This emphasizes the destructive nature of Modic changes.
In May of 2013, an article in Advances In Orthopedics indicated surgical dynamic stabilization was an effective treatment for Modic type 1 and 2 degenerative symptoms, indicating the unstable nature produced by Modic changes. Therefore, there are options to using antibiotics related to Modic changes, however, more research is being done.
There have been studies indicating various experimental compounds like IS0-1 or macrophage migration inhibitory factor antagonist can reduce inflammation associated with Modic type 1 changes, therefore, exerting potent effects therapeutically, as indicated in a February 2014 issue of Clinical Orthopaedics and Related Research. There are other potential drugs, studies and experiments ongoing, however, at this time, using antibiotics for back pain related to Modic 1 changes seems the most promising, cost effective and poses the least amount of risk.
The authors of a May, 2014 article published in the journal Neuroradiology performed a study with Modic Type 1 patients using vertebroplasty, where they injected bone cement to treat their low back pain. They noted most patients improved within 4 weeks, while others showed a gradual improvement at 6 months and 1 year. They indicated this procedure to be effective as a therapeutic option for those back pain sufferers who do not respond to conservative treatments, with clearly defined Modic 1 degeneration of the low back.
BMC announced in Trials, Apr 9, 2014, a study that will use the drug pamidronate, a bisphosphonate in the same class as zoledronic acid, for Modic type 1 changes. They noted that if the primary goal is not achieved, the patients will be offered either a rigid or partially rigid back brace, indicating the unstable nature of Modic 1 changes. They describe Modic changes using a largely French terminology as erosive degenerative disc disease (EDDD), however, they have recently changed it to active discopathy.
A 2019 study in The Spine Journal used radiofrequency ablation of the basivertebral nerve, a minimally invasive treatment, for patients with Modic Type 1 or 2 vertebral endplate changes. The authors found it to provide significant improvement of pain and function at 3 months compared to standard care.
Radiofrequency ablation uses a microelectrode through an inserted needle to heat the offending nerve to stop it from sending pain signals. This procedure is also used for facet joint pain and sacroiliac joint pain. The study did not indicate the pain was due to Modic changes by current objective and subjective criteria other than MRI documented changes, and listed as “suspected vertebrogenic chronic low back pain”.
A 2021 report in The Journal of Medical Investigation indicates when Modic I changes inflammation is intractable to other methods, surgical intervention is often recommended. The typical procedure is segmental fusion. However, this may cause the adjacent degeneration; thus, motion preservation surgery is recommended if possible. The study reports a motion preservation full-endoscopic intradiscal debridement and drainage surgery under the local anesthesia. They call it transforaminal full-endoscopic disc cleaning surgery (FEDC).
Although effective for the patient, the problem I see is that they tried conservative treatment for a year consisting of intra-venous injection of steroids, oral NSAID’s for one year and antibiotics for three months. The antibiotic protocol is not indicated. No intradiscal steroid injection was performed.
A 2022 study in Pain Physician indicates studies demonstrate a strong innervation of the vertebral endplates by the basivertebral nerve. The authors indicate that basivertebral nerve ablation might be a promising treatment for chronic low back pain in patients exhibiting Modic type 1 or 2 endplate changes.
It is very nice to see such attention to Modic changes in scientific literature. Results of some of these studies are impressive, however, I am somewhat perplexed at the lack of further studies using antibiotics. Regardless, there are some options to treating back pain with antibiotics for Modic 1 changes, although, more invasive or using drugs with more significant side effects. I see no reason to avoid using the least invasive method as a starting point, however, for those who are not able to take antibiotics, some options seem viable.
So, Modic type 1 changes, regardless of the cause, are an indication of active, inflammatory degeneration and biomechanical instability associated with poor responses to generally recommended treatment guidelines. Modic changes represent a dynamic condition, with type 1 being strongly associated with back pain and reflecting a state of active and rapidly progressing degenerative disc disease. They can increase in size or perhaps convert into type 2 changes, which are less associated with back pain, however, further structural problems or stresses may cause a conversion back into type 1 changes. Conversion may also lead to type 3 changes, representing a more stable situation, however, these may convert back into type 2 and subsequently type 1.
Therefore, this can be very frustrating for those of us that have this condition; both myself and those who come to me for advice. In my experience, response by the general and specialist medical community is not good, and I am being polite. Most are either unaware, too set in their ways, too concerned with what their colleagues, bosses or insurance companies will think, or just react emotionally to the prospect of Modic 1 changes being a distinct entity or possibly related to an infectious process. It is clear, however, that recent years of research have proven this to be a distinct disease process and not a finding related to “normal aging”. Perhaps there is just a lapse of time between research results and practical application.
One must discern the possibility that if antibiotic responsive bacterial infection represents a significant percentage of Modic 1 changes and related medical problems regarding pain and disability; then some of the procedures currently performed, including services for rehabilitation and management of chronic pain as well as psychological therapies could become unnecessary. Great for patients and reducing medical costs, however, it would pose a significant economical disadvantage for some doctors as well as related services performed by hospitals, clinics and rehab centers.
Conversely, non-infectious, symptomatic Modic 1 changes could respond better to new therapies, such as biocement injections that more specifically target the problem, providing better therapeutic outcomes and less invasive procedures.
Having documented extensively on Modic changes and antibiotic therapy at NeckSolutions, I have looked at Chiropractic Management Of Modic Changes, from the perspective of taking and successfully passing the certification course in Modic Antibiotic Spinal Therapy by Dr. Albert.
Are My Modic 1 Changes Caused By Bacteria?
Not all Modic Type 1 changes are caused by bacterial infection. There are mechanical Modic changes that are not infected with bacteria. The way to tell if your Modic Type 1 changes are caused by a bacterial infection is to have a Diffusion Weighted MRI scan, which is an extra parameter done during the exam, nothing invasive. This method is not 100%, but has been shown to be very effective in determining infectious from strictly degenerative or mechanical Modic 1 changes. Diffusion weighted MRI is not standard MRI procedure for back pain, it is used to look more specifically for more aggressive disease processes.
In a April 2014 edition of the American Journal of Neuroradiology, the authors did a study with Diffuse Weighted MRI to differentiate infectious from degenerative Modic 1 changes. When a signal called a claw sign was clearly or probably identified, there was an 84 to 100% indication of no infection. An absence of the sign, with indication of a diffuse signal pattern, indicated a 93 to 100% chance of infection related Modic 1 changes.
This clearly gives an indication that Diffusion Weighted MRI may distinguish infection from strictly degenerative or mechanical Modic changes. Therefore, absence of the claw sign would be an indication that antibiotics may be beneficial in treating Modic 1 changes. A distinct claw sign would not completely contraindicate the use of antibiotics for back pain, however, it would indicate the favorability of other methods to stabilize the Modic 1 changes, as indicated above and as research in the future might indicate.
So, Modic changes can be a result of stress from shearing type forces in the lower back, which are strictly mechanical in nature and not related to a bacterial infection. Advances in imaging like DWMRI can help define if antibiotics should be the primary mode of treatment. Some choose biopsy. In general, I see about 30-40% of Modic 1 changes are related to bacterial infection. Methods to help differentiate the 2 could improve results regardless of cause, albeit at a cost.
From personal communication with Lawrence Tanenbaum, MD, one of the authors of this study, it was indicated that “… the claw represents a border zone induration as a response to a slow degenerative process. Infection is presumed to advance more rapidly and thus not manifest the striking border zone changes. I would assume it applies to all infections but more experience is needed.” This brings up the questions if Modic 1 changes due to infections progress at a more rapid rate than Modic 1 changes that are only structurally related to the degenerative process. Always a humbling experience corresponding with some of the great minds in research. As Dr. Adams reminds me “… Modic changes are too common to be a reliable guide to disc infection on their own.”
In the July, 2014 edition of the Journal of Neuroimaging, the authors did a study using Diffusion Weighted MRI with Coefficient Mapping and determined its usefulness in diagnosing early disc infection (infectious spondylodiscitis).
A 2018 study in the Journal of Spine Surgery found MRI with diffusion is useful to differentiate patients with type I changes due to degenerative disease with (claw sign) or type I changes due to infection (absent claw sign).
Therefore, there is no longer any excuse for guessing. However; from my experience, insurance companies are very reluctant to pay for DWMRI with this diagnosis. Hopefully, studies will incorporate this method into their criteria for better patient selection and results.
A study in a 2007 issue of Arthritis & Rheumatism, showed in those with chronic back pain, low grade inflammation as indicated by high-sensitivity C-reactive protein (hsCRP) levels could point to Modic I changes. Now, I have not seen additional studies confirming this.
Is The Spinal Disc Only Affected With These Bacteria?
In an April, 2013 edition of the Journal of Shoulder and Elbow Surgery, noted P acnes, the same bacteria involved with infectious Modic 1 changes, in cultures of the shoulder joint in patients having shoulder replacement due to joint disease without having any signs of infection.
They found about 40% had bacteria in the joint fluid as well as tissues taken prior to the insertion of the implants. The authors indicate a possible role of the bacteria P. acnes in the cause of shoulder joint disease, representing a low-grade infection that has been present but unrecognized prior to the operation.
A 2014 edition of the same journal noted 56% of those undergoing primary shoulder arthroscopy were infected with P. acnes. The authors suspect this was from skin contamination.
Is Using Antibiotics For Back Pain New?
Actually, No. Antibiotics have been used in treating arthritis, including back pain symptoms for about 70 years! Sulfasalazine, also called by the name Azulfidine, has been used for symptoms of arthritis stiffness, pain & swelling. It is a sulfa drug that combines salicylate, which is the main chemical in aspirin, along with a sulfa antibiotic. Sulfasalazine decreases pain and swelling associated with arthritis, and may act to prevent joint damage and can possibly decrease the risks of long-term loss of function.
Sulfasalazine was initially used to treat rheumatoid arthritis over 70 years ago. It was once thought that rheumatoid arthritis was caused by bacterial infection. The drug was developed to combine the aspirin like anti-inflammatory with an antibiotic containing sulfa. Antibiotics can be Gantrisin, Septra, Bactrim and others. Now, it is not believed that bacteria causes rheumatoid arthritis, but sulfasalazine is still used alone or in combination with other drugs, depending on symptom severity. It is not quite understood how this works for rheumatoid arthritis, but it can take 1 – 3 months before noticing improvement. So, using antibiotics for back pain is not new, however, using them specifically for Modic changes called antibiotic spinal therapy is.
