Cervical Myelopathy – Spinal Cord Compression
Neck pain due to cervical spine and related disorders is a common and often debilitating problem and an important reason for seeking medical attention. It often arises without relation to a specific activity or neck trauma. Such is often the case with cervical myelopathy.
We will consider what is often termed cervical spondylotic myelopathy which is a degenerative spine condition with symptoms of neck pain, numb and/or clumsy hands, gait difficulties, sphincter dysfunction, and impotence. We will be somewhat repetitive with symptoms, however, it is important to recognize some of the early indications and be aware of the different findings as many of the symptoms are typically not associated with neck problems. Progressing or advancing symptoms most often require a surgical consultation.
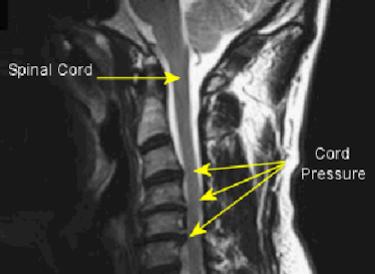
We detailed degenerative disc disease, cervical spondylosis, cervical degenerative disc disease and disc herniation in a previous articles. Unfortunately, the result of this degenerative process may involve myelopathy – pressure on the spinal cord.
 Cervical spondylotic myelopathy is the result of narrowing (stenosis) of the cervical spinal canal by degenerative and/or congenital (formed at birth) changes. Degenerative myelopathy is the most common type of spinal cord dysfunction in patients older than 55 years. The onset is usually subtle, with long periods of fixed disability and episodic worsening. The first sign is commonly gait spasticity or difficulty in walking, followed by upper extremity numbness and loss of fine motor control in the hands.
Cervical spondylotic myelopathy is the result of narrowing (stenosis) of the cervical spinal canal by degenerative and/or congenital (formed at birth) changes. Degenerative myelopathy is the most common type of spinal cord dysfunction in patients older than 55 years. The onset is usually subtle, with long periods of fixed disability and episodic worsening. The first sign is commonly gait spasticity or difficulty in walking, followed by upper extremity numbness and loss of fine motor control in the hands.
It begins with disc degeneration, which may cause segmental instability and hypertrophy (outgrowths) of vertebrae and facet joints. As this develops, disc spaces become narrowed gradually. Severe disc degeneration can be defined as disc height less than half normal disc height. After severe disc degeneration develops, neighboring discs may sustain increased stress and the biomechanics of cervical spine is changed. Severe disc degeneration is equivalent to an autofusion (fuses on its own) as a compensation process for segmental instability. The mechanical factors involved are divided into two groups: static and dynamic.
Factors Related To Cervical Myelopathy
- A 2023 study in the Asian Spine Journal indicates the problem includes spinal cord structure and function abnormalities caused by both static and dynamic factors.
1) Static factors include: congenital spinal canal stenosis, disc herniation – central type herniations, osteophyte (bony outgrowths or arthritic spurs) of the spinal bones, degenerative outgrowth of the uncovertebral joints at the back of the spinal bones and facet joints, hypertrophy (thickening) of ligaments along the spine (flavum and posterior longitudinal ligaments).
2) Dynamic factors are abnormal forces placed on the spinal column and spinal cord during flexion (bending head forward) and extension (bending head backward) of the cervical spine. An example would be the trauma caused to the spinal cord by repetitively being compressed against a degenerative outgrowth during normal flexion and extension of the cervical spine. Mechanical compression of nerve tissue is only one of the pathologic mechanisms. Another is spinal cord ischemia, which happens when degenerative elements compress blood vessels that supply the spinal cord and nerve roots.
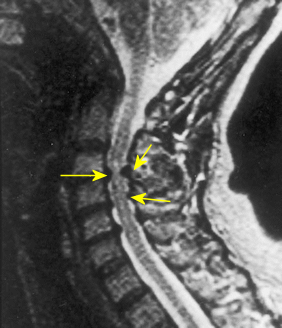 The spinal canal houses the spinal cord and the immediate portion of the cervical nerve roots. Stenosis is a condition of narrowing. Where the spinal cord normally has sufficient room, stenosis may cause a narrowing of the spinal canal leading to spinal cord compression. Typically, this stenosis is from degenerative changes, a herniated disc, and one may have a predisposition from a congenitally narrowed spinal canal which is genetic.
The spinal canal houses the spinal cord and the immediate portion of the cervical nerve roots. Stenosis is a condition of narrowing. Where the spinal cord normally has sufficient room, stenosis may cause a narrowing of the spinal canal leading to spinal cord compression. Typically, this stenosis is from degenerative changes, a herniated disc, and one may have a predisposition from a congenitally narrowed spinal canal which is genetic.
This narrowing in the lower back (lumbar canal stenosis) may produce only radiculopathy (pinched nerve) because the tip of the spinal cord called the conus medullaris is at the level of L1-L2, however, other leg symptoms may occur. Cervical (neck) canal stenosis can produce a sometimes complex picture of cervical myelopathy and radiculopathy.
Proprioception is also impaired. Proprioception describes the sensations generated within the body that contribute to awareness of the relative orientations of body parts, which are fundamental to the normal control of human movement. Therefore, myelopathy can cause impairment of postural stability.
With pressure on the spinal cord, there is a compromise of the blood vessels and the symptoms vary depending on the site of this ischemic damage to the cord. Patients often complain of clumsy or weak hands or feet that may be hypersensitive. Tingling fingers and leg stiffness are also common complaints. Examination may reveal deep touch, vibration, joint movement awareness and the ability to sense 2 points on the skin surface may be disturbed. Patients may claim they cannot feel a cold floor or hot water in the tub. There may also be spasticity with weakness of the upper or lower extremities. Movements may slow down, finger extension may be incomplete, and wrist extension may be exaggerated.
Symptoms
- In a 2004 study published in the journal SPINE, the most common symptoms of 79 patients with degenerative cervical myelopathy were: Numb arms or hands 91% | Numb legs or feet 85% | Clumsy hands 82% | Neck pain 78%
Symptoms can include: Pain in the neck, subscapular area, or shoulder. Numbness or altered sensations in the upper extremities. These are usually nonspecific, although specific sensory complaints can occur from a coexisting pinched nerve or radiculopathy. Sensory changes in the lower extremities. Motor weakness in the upper or lower extremities. Gait difficulties. Many patients have what is called a spastic gait which is a broad-based, hesitant, and jerky movement, compared with the smooth rhythmic normal gait.
- A 2020 study in Clinical Spine Surgery found the most common chief complaint was upper extremity sensory (pain, numbness) while the most common overall symptom were upper and lower extremity sensory or motor function deficits, about 80%. Neck pain as an overall complaint was over 55% among these select surgical cases (484 patients).
Some studies have indicated that a subtle gait disturbance is the most common presentation. Bowel and bladder dysfunction is also common. A study in a series of 269 patients, bowel dysfunction was observed in 15% and bladder dysfunction was observed in 18%. Other studies have found that 20% of their patients with degenerative myelopathy over age 65 had bladder dysfunction, mostly associated with urinary retention.

Patients with cervical disorders of one type or another may present with lower extremity and bladder or bowel symptoms often with only minimal neck pain. Therefore, the neck may have symptoms referable to lower extremities as well as bladder and bowel functions, altered sensation in the lower extremities, weakness of the lower extremities, gait disorders, impotence in men, and anorgasmia in women.
- In a 2006 study in the journal SPINE, symptoms of impotence in men were improved after surgical treatment of myelopathy.
- A 2011 study in the European Spine Journal gives an idea of the presentation of leg pain in myelopathy of the cervical spine that has been corroborated by other authors. It is typically called Funicular pain related to the spinal cord compression and is often described as “sciatica like pain“.
There is a diffuse or more widespread picture of disturbance rather than a dermatomal type, which is more circumscribed to particular areas.. The pain tends to be constant, burning, and involving the lower extremity. It may be described as cold with tightness and is ascending or from the bottom up rather than typical radicular pain, which is descending or downward as in a pinched nerve or herniated disc.
- A 2020 study in Pain Research & Management noted that 31% of those with myelopathy related to cervical spondylosis experienced headaches. The authors indicated they were cervicogenic headaches and a result of nerve damage or a malfunctioning nervous system. A portion were able to be relieved with decompression surgery, with worse outcomes in those with more severe pain and lower quality of life scores.
- A 2022 study in The Spine Journal notes patients with degenerative myelopathy of the cervical spine exhibit postural instability compared with healthy adults. This results from a complex impairment in proprioception and somatosensory system integration controlled by the neural tract in the spinal cord. When a sensory system is impaired, other sensory systems may over-activate to compensate. The authors indicate patients may require balance training and posture education after surgery.
It is important to get a complete examination and for a qualified health care professional to differentiate a peripheral neuropathy, cauda equina syndrome, and myelopathy. To further illustrate the importance of a thorough examination, although the names may be unfamiliar, the differential diagnosis (other conditions which may present similar symptoms) includes multiple sclerosis, transverse myelitis, progressive motor neuron disease, subacute combined degeneration, syringomyelia, spinal cord tumors, cerebral hemisphere disease, peripheral neuropathy and normal pressure hydrocephalus. It may also be related to dropped head syndrome.
- The Japanese Orthopaedic Association developed a scoring system for cervical myelopathy:
I Motor function of the upper limbs
– 4 Normal
– 3 Able to eat using chopsticks with slight difficulty
– 2 Able to eat using chopsticks with difficulty
– 1 Able to eat using a spoon only
– 0 Unable to eat unaided
II Motor function of the lower limbs
– 4 Normal
– 3 Able to walk without support with slight difficulty
– 2 Able to walk up and down stairs only with support
– 1 Requires support to walk even on level ground
– 0 Unable to walk
III Sensory function (same in upper and lower limbs, and trunk)
– 2 Normal
– 1 Slight sensory disturbance or numbness
– 0 Distinct sensory disturbance
IV Bladder function
– 3 Normal
– 2 Slight urination difficulty (pollakisuria, retardation)
– 1 Serious urination difficulty (residual urine, dysuria)
– 0 Urine retention
Additional findings: Muscular tone in the legs will be increased, Deep tendon reflexes in the knee and ankle will be accentuated (hyperreflexia), Forced extension of the ankle may cause the foot to beat up and down rapidly (clonus), Scratching the sole of the foot may cause the big toe to go up (Babinski reflex) instead of down (normal reflex), Flicking the middle finger may cause the thumb and index finger to flex (Hoffman’s reflex), Compromised coordination may be evidenced by difficulty walking placing one foot in front of the other (tandem walking).
Shooting pains into the arms and legs like an electrical shock, especially when bending the head forward (neck flexion) is known as Lermitte’s sign. Neck flexion can produce paresthesia (altered sensations), usually in the back, but sometimes into the extremities. Lhermitte’s sign is most commonly associated with an inflammatory process such as multiple sclerosis, but it is sometimes noted with spinal cord compression.
- A 2002 study in the journal Spine, noted a dispositional factor that possibly contributes to the prevalence of cervical myelopathy in males. Assessment of the cervical spine radiographs of healthy young adults revealed that the cervical canal/body ratio (size of the spinal canal to vertebral body) was significantly larger in women than in men. The incidence of canal stenosis was 19.4% for men and 4.4% for women. The discrepancy of the canal/body ratio in adulthood was attributed to the growth spurt of the male vertebral body at puberty.
- Many studies have been done to find out relationships and risk factors without significant conclusions. A 2014 study in the Spine Journal found that cord compression in combination with vertical spinal cord motion contributes to deterioration in cervical myelopathy.
You should have an understanding of the causes and symptoms. It is important to understand that neck problems may cause symptoms that extend beyond a local area and recognize these symptoms in yourself and others so that prompt attention can be addressed. While home care products can help with relief; the worse the symptoms, the more likely surgery is necessary and there may be negative consequences for delay.
- A 2019 study in European Radiology found some disturbing complications of myelopathy from cervical spondylosis in that it leads to brain damage affecting the white and gray matter of the cortex resulting in brain atrophy and functional adaptive changes from prolonged cervical spine compression.
- A 2019 study in the Journal of Neurosurgical Sciences found those undergoing spinal fusion for cervical myelopathy had a high prevalence of Vitamin D deficiency, which was associated with greater disability and worse outcomes. If your levels are less than 30 ng/mL, vitamin D supplementation may be a wise choice.
- A 2020 review and analysis in the Journal of Orthopaedic Science compared 2 methods of surgery for cervical spondylotic myelopathy. They found anterior decompression with fusion (ADF) better preserved the cervical lordosis than laminoplasty, which can have better long term outcomes, however, it was associated with a higher incidence of surgical complications.
- A 2020 study in the Journal Neurosurgery Spine found residual numbness of the upper extremity was present in 41% of patients undergoing cervical posterior decompression surgery for at least 2 years. Female and preoperative severe upper extremity pain were predictive factors and neck pain improved significantly less.
- According to a 2020 article in American Family Physician degenerative cervical myelopathy is a collection of conditions that result in progressive spinal cord dysfunction due to cord compression. Patients are typically male, where there is a 3:1 male-to-female ratio, and the average age at presentation is 64 years. The authors indicate surgery is recommended for those with moderate to severe symptoms or rapidly progressive disease, while conservative treatments with monitoring may be considered in patients with mild to moderate disease.
- A 2021 report in the British Journal of Neurosurgery indicates fever may be a rare symptom of degenerative myelopathy of the cervical spine, which may be a special manifestation of sympathetic nerve stimulation or autonomic dysfunction by chronic compression of spinal cord.
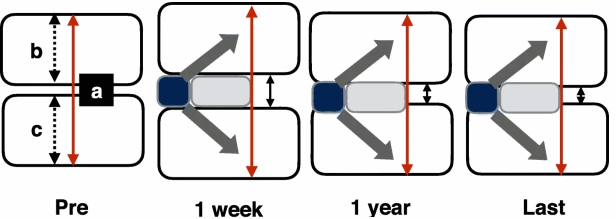
- A 2021 study in BMC Musculoskeletal Disorders found after anterior cervical decompression and fusion (ACDF) surgery, “If postoperative IH [intervertebral space height] changes are maintained at 2 to 4 mm after a year, a satisfactory imaging parameters and relatively low complications may be achieved after ACDF surgery using a zero-profile device.
- A 2021 study in Neurosurgery found for degenerative myelopathy, surgery obtained significant improvements in neck, headache and arm pain. 44.6% experienced complete recovery or felt much better at 1 year. 27.7% experienced adverse effects within 3 months.
- A 2022 study in Life (Basel) found those with degenerative myelopathy had greater disturbances in concentration related activities, like reading, focusing, driving, sleeping, and resting compared to those with disc pathologies.

 Neck Traction Devices
Neck Traction Devices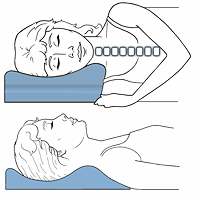 Cervical Pillows
Cervical Pillows Neck Support Collars
Neck Support Collars Muscle Therapy Tools
Muscle Therapy Tools Head Supports
Head Supports Topical Pain Relievers
Topical Pain Relievers Special Pillows
Special Pillows Heat Therapy
Heat Therapy Cold Therapy
Cold Therapy TENS Therapy
TENS Therapy Posture Braces
Posture Braces Neck Stabilization
Neck Stabilization Ergonomic Aids
Ergonomic Aids New Mattresses
New Mattresses Relief Supplements
Relief Supplements