Neck Related Headaches: Head Pain Referred From The Neck – Cervicogenic Headache
Headaches due to neck problems are called neck related or cervicogenic headaches. The joints, discs, muscles, and ligaments of the neck all contain nerve endings which are sensitive to neck injury or strains that can result in headaches.
The pain of cervicogenic headaches is usually worse at the base of the skull, and may spread to the forehead, temples, eyes, face and shoulder. Poor neck posture in moving your neck and/or holding your head and neck in one position for long periods may bring on the pain or make it worse. Neck muscles become stiff or tender and there may be abnormal findings on neck X-rays.
| Headaches | Neck Related Headaches | Tension Headaches | Migraine Headaches |
| Pain Severity | Mild to Moderate – Sometimes Severe | Mild to Moderate | Mild to Severe |
| Pain Location | Usually One Side | Usually Both Sides | Usually One Side |
| Family History | No | No | Yes |
| Nausea | Sometimes | Sometimes | Yes |
| Vomiting | No | No | Yes |
| Aura | No | No | Sometimes |
 Additional symptoms of neck related cervicogenic headaches include nausea, vomiting, sensitivity to noise or bright lights, dizziness, blurred vision, or difficulty swallowing. It is sometimes difficult to be sure of the headache type because these same symptoms can also be part of migraine headaches. Sometimes people with tension or migraine headaches may also have cervicogenic headaches and may respond to treatments of the neck.
Additional symptoms of neck related cervicogenic headaches include nausea, vomiting, sensitivity to noise or bright lights, dizziness, blurred vision, or difficulty swallowing. It is sometimes difficult to be sure of the headache type because these same symptoms can also be part of migraine headaches. Sometimes people with tension or migraine headaches may also have cervicogenic headaches and may respond to treatments of the neck.
One study indicated that cervicogenic headaches were diagnosed in at least 18 percent of people with more than four headaches per month and 2.5 percent of the population as a whole. Additional studies found that diagnoses in 14 percent of people with frequent headaches and 16 percent of people with chronic headaches.
In a 2020 review in the journal Cephalalgia the authors indicate the criteria for cervicogenic headaches should also include precipitation of pain by digital pressure on neck trigger points and specific movements, strictly one-sided pain, diffuse one sided shoulder and arm pain, and pain that starts in the back and moves forward.
Causes
There are structures in the neck that are causative; most commonly problems with the discs or facet joints of the upper and middle part neck are often involved with injury, arthritis and postural stress, while muscle strain may add to the overall pain.
Disc Problems
Discs in the neck provide much of the stability for the bones above and below them. The outer layer of the disc (anulus) has a very rich nerve supply that can be irritated if the disc develops tears or cracks. The anulus can be injured by a trauma, such as whiplash or by chronic strain due to poor posture. Tears in the outer portion of the disc cause inflammation and even the weight of the head puts more pressure on the weakened disc and causes more pain.
Facet Joints
The facet joints can also be a cause of headaches. When these joints begin to wear, they may pop or crack, however, these noises are not dangerous.
The joints contain cartilage and a rich supply of nerves, and they can wear down, become inflamed, and start hurting similar to other joints of the body. In a medical procedure called radiofrequency neurotomy, the pain can often be helped for 6 to 18 months by applying heat to the nerve. This is often used in cases of cervical facet syndrome and can be seen in cases of chronic whiplash.
Atlanto Occipital and Atlanto Axial Joints
Where the skull and neck meet at the top of the neck is a joint called the atlanto occiptial joint (A-O joint). The next joint down is called the atlanto axial joint (A-A joint). These joints do not have discs or facets, but either can become inflamed and cause pain and both joints are vulnerable to whiplash injury. Chronic neck pain and headaches from these joints may respond well posture modifications and retraction neck exercises. Additionally, Chiropractic adjustments may be helpful.
A 2021 study in Pain Medicine used diagnostic blocks to the synovial joints of the cervical spine to find that in those with headache greater than neck pain, the C2/3 joint was the source in 62%, with C1/2 (7%) and C3/4 (6%). In those with headache less severe than neck pain, C2/3 was the source in 42%, with lower cervical joints in 18% and the C3/4 joint in 7%.
Muscle and Ligament Injury
Nearly two-thirds of recurring headaches are associated with muscle stiffness or spams, however, the muscles are most often not the main cause of pain. Pressure on neck muscles can cause pain, however, this also puts pressure on the facet joints lying under the muscle, so it is not always possible to identify the direct cause of the tenderness.
A 2018 study in the journal Physiotherapy Canada found that higher sensitivity of trigger points in the upper trapezius muscle can be used as a differential diagnostic factor for cervicogenic headaches. The authors concluded, “This finding emphasizes the importance of integrating this muscle into the rehabilitation programs of patients with cervicogenic headache”. This condition is often found with trapezius myalgia, and we have a specific rehabilitation program at the link.
A 2023 study used trapezius muscle fascia blocks, which were effective in reducing neck related disability and medication consumption for cervicogeneic headaches, indicating a focus on this muscle and trapezius myalgia for symptomatic relief and functional improvement.
As a result of injury to a disc or facet joint, neck muscles may go into spasm adding to the overall pain. Discs and facet joints are far more vulnerable to injury and far more likely to cause chronic neck pain than muscles and ligaments.
Occipital Neuralgia
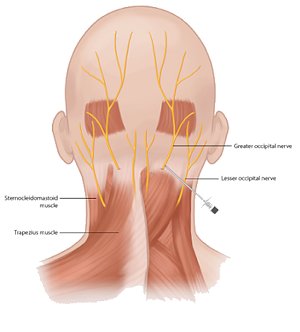 The greater occipital nerve along with the lesser is located at the base of the skull and runs through deep and superficial muscles and fascia of the neck. Although not a common primary cause, in many people with cervicogenic headaches, this muscle is tender and the nerve may be irritated. It can be injured in whiplash where a relatively stable muscle like the obliquus capitis inferior can act as a tether to strain the nerve during traumatic events as indicated in 2019 Plastic and Reconstructive Surgery study.
The greater occipital nerve along with the lesser is located at the base of the skull and runs through deep and superficial muscles and fascia of the neck. Although not a common primary cause, in many people with cervicogenic headaches, this muscle is tender and the nerve may be irritated. It can be injured in whiplash where a relatively stable muscle like the obliquus capitis inferior can act as a tether to strain the nerve during traumatic events as indicated in 2019 Plastic and Reconstructive Surgery study.
There may be a pulsating type of pain since there is an artery that runs around the nerve. It may sometimes be aggravated by motions of the neck like rotating and bending. If a local anesthetic is injected into the muscle and around the nerve, the headaches may improve. The anesthetic can provide immediate relief and, if combined with a steroid, further improvement may be noted in 3-5. On occasion, doctors perform surgery to relieve the pressure on the nerve, however the results are not very predictable.
A 2020 study in the journal Cephalalgia found that patients with less sensitivity to cervical area palpation (manual pressure) and were headache free on the day of the intervention had better results after a greater occipital nerve block.
Treatment of Neck Related Headaches
Changing or avoiding postures or activities that seem to precipitate headaches is an important first step. Once a headache is established, specific postures may relieve pressure on your neck. Employing a ergonomic strategies at work and home is part a good long term solution.
Posture
Proper neck posture means alignment of the head and neck to minimize the forces on the discs, facet joints and other structures. Bad posture, especially when sitting for prolonged periods, is one of the most common causes of neck headaches and improving posture often improves pain. Poor posture places strain on the discs and joints and causes pain. Strategies to reduce forward head posture can be beneficial.
A 2020 study in Musculoskeletal Science and Practice found alterations of the thoracic and lumbar spine corresponded to an increased odds of suffering from cervicogenic headache.
Good neck posture is also related to good low back posture. It is necessary to sit straight and allow your back to keep its normal curve to balance the rest of the spine. Forward bending should occur mostly at the base of the skull, not the lower back.
Exercises
With the head and neck aligned and balanced, the muscles and ligaments have minimal stress and strain. It is nearly impossible to be in perfect posture all of the time, so the muscles and ligaments must partially support the head and neck. Conditioned muscles are more able to hold the head and neck in proper position and are essential to good posture.
A 2022 study in PM & R found manual therapy in the short term and neck exercise in the long term may be efficacious to treat adults with cervicogenic headache.
A 2023 study in Musculoskeletal Science & Practice therapeutic exercise may achieve clinically relevant reductions in headache frequency, intensity, and disability for patients suffering from headache due to the neck issues.
Medications
The most useful over the counter medications are acetaminophen, ibuprofen, and naproxen. There are much stronger medications that can be helpful, but they require a doctor’s prescription. Diagnosis of the type of headache is important for effective treatment through medications.
Injections
There are several types of injections that can be helpful for neck related headaches. There are two major categories of therapeutic injections; steroid injections and injections that heat or freeze a nerve (neurotomy) to stop it from conducting pain.
For treatment resistant cases, a 2019 study in the journal Neurological Sciences demonstrated that combining pulsed radiofrequency of the C2 dorsal root ganglion with epidural steroid injections provided sustained relief of pain symptom and improved quality of life in a case control study of 139 patients.
A 2020 study in the Clinical Journal of Pain found that in 57 patients with intractable cervicogenic headache, pulsed radiofrequency treatment targeting the mid-cervical medial branches resulted in a satisfactory, long lasting results without serious complications.
A 2021 review indicates greater occipital nerve block to be a useful method of treatment in various headache disorders as it shows early effects in reducing the pain severity, long term effect following a single injection, easy technique that is minimally invasive, low adverse reactions and reasonable cost.
Surgery
Surgery should be the last thing to consider for treating neck related headaches, but it can be helpful in patients with severe pain who have not responded to other treatments. Sophisticated testing with X-rays, MRI scans, facet joint injections, and discography is necessary to determine the best surgical options.
 TENS Therapy TENS Therapy |
 Posture Braces Posture Braces |
 Neck Stabilization Neck Stabilization |
Conclusion:
Modification of posture and relief of inflammation using non-surgical or injection methods are the most practical and can help in most cases. Choosing a good pillow, using an effective home neck traction device along with specific cervico-cranial exercises and supplements can improve the neck in both structure and function to help in the relief of headaches that may be related to the neck. Another natural alternative for headache relief is the headache pressure point located on the hand.
A 2021 review in the Korean Journal of Anesthesiology indicates for those who do not respond to the above conservative measures; occipital nerve block, atlantoaxial joint injection, cervical facet joint injections, cervical epidural steroid injection, and deep cervical plexus blocks can be considered reasonable options. Radiofrequency neurotomy can achieve long term favorable outcomes, with pulsed therapy showing better safety than conventional radiofrequency.
For more on neck related headaches, see the headache neck pain article.

 Neck Traction Devices
Neck Traction Devices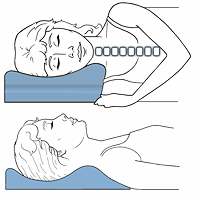 Cervical Pillows
Cervical Pillows Muscle Therapy Tools
Muscle Therapy Tools