Dropped Head Syndrome Results In Neck Pain, Trouble Eating & Interferes With Vision
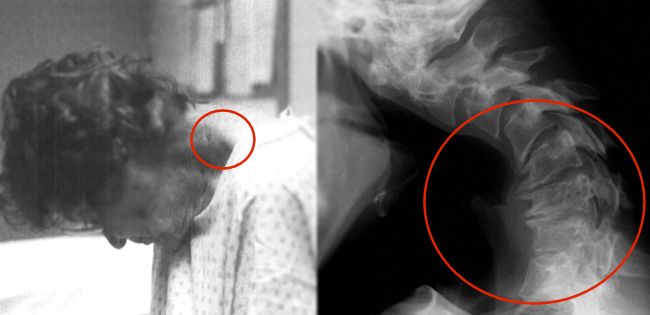
Dropped head syndrome causes a recognizable deformity with varying degrees of “chin on chest” posture. There is usually weakness of the neck muscles that results in the head dropping forward, sometimes called ptosis of the head. The fixed flexion or forward bending of the neck is often painful, interferes with feeding and horizontal eye gaze. The head is typically able to be passively ranged or moved up by hand.
 It is most often associated with problems of the nerves and/or muscles, however; in some cases there is no obvious cause even after extensive evaluation, or muscle biopsy may indicate a cause that is isolated to the neck extensor muscles and non-inflammatory. These cases are called isolated neck extensor myopathy or may be described as idiopathic head ptosis, where neck muscle weakness is the only symptom.
It is most often associated with problems of the nerves and/or muscles, however; in some cases there is no obvious cause even after extensive evaluation, or muscle biopsy may indicate a cause that is isolated to the neck extensor muscles and non-inflammatory. These cases are called isolated neck extensor myopathy or may be described as idiopathic head ptosis, where neck muscle weakness is the only symptom.
There are many potential and varied causes: central or peripheral nerve disorders like myasthenia gravis or Parkinson’s disease, autoimmune problems of muscle and connective tissue such as polymyositis and systemic sclerosis; they may be systemic and progressive with a poor prognosis like amyotrophic lateral sclerosis (ALS).
The most common cause of dropped head syndrome is isolated neck extensor myopathy and may have a benign clinical course.
The 4 Most Common Causes Of Dropped Head Syndrome
- A 2019 systematic review in Clinical Spine Surgery lists the top 20 causes. Of these, 4 stand out as the most common – with approximate percentages.
- Isolated Neck Extensory Myopathy (32%)
- Parkinson’s Disease (20%)
- Myasthenia Gravis (12%)
- Amyotrophic Lateral Sclerosis (7%)
Finishing out the remaining (28%) of the top 20 causes of dropped head syndrome in descending order of prevalence as above. The percentages are not included, but decline rapidly from 5% to 1%:
- MEK inhibitor
- Endocrine/Electrolyte Abnormality
- Postradiation
- Scleroderma
- Polymyositis
- Postoperative Myopathy
- Spinal Cord Injury
- Amyloidosis
- Anti-GAD (Gadolinium) Inflammatory Myopathy
- Lipid Storage Disease
- Neuroendocrine Tumor
- Neurofibromatosis Type 1
- Inflammatory Polyneuropathy
- Cervical Myelopathy
- Polio
- Stroke
- Vasculitis
Treatment For Dropped Head Syndrome
It is both a challenging and complex condition to diagnose and treat. Management necessitates comprehensive multi-disciplinary diagnosis to ascertain the primary cause. Many of the conditions are medically treatable and it is possible that the deformity can be decreased to an acceptable level. Conditions like Parkinson disease, inflammatory myositis, and secondary myopathies related to endocrine or metabolic dysfunction may show substantial improvement with medications. Other causes resulting in structural changes like radiation fibrosis may respond poorly to medical treatment.
The best treatment methods are often vague and based on case reports. For symptoms that persist even with treatment of an underlying pathology, steroids, bracing and strengthening exercises with other conservative forms of physiotherapy are suggested and surgical options as a viable last resort.
- According to a 2020 study in the Journal of Orthopaedic Surgery, sufficient conservative treatment is essential and surgical indications should be carefully determined.
- A 2022 study in the Journal of Clinical Neuroscience uses a short and intensive rehabilitation (SHAiR) program consisting of cervical muscle exercise, range of motion exercise, neck and and back mobilization, hip lift exercise, anterior pelvic tilt exercise, and walking exercise can be an effective therapy.
Supports/Bracing
Options for orthotic stabilization and varying degrees of correction of dropped head syndrome include removable hard or soft collars, corset or vest combinations, banding systems, and special wheelchair headrests. While some may offer a type of nuromuscular re-education toward correction or prevention of atrophy, these devices are often only a temporary or partial solutions, achieving long term satisfaction only in select patients. However, they can help maintain horizontal gaze/eye contact, assist in proper feeding, facilitate other daily living activities and improve quality of life.
While head supports may be cumbersome, irritate the skin, and may cause further deconditioning or deterioration of neck muscles, they should be instituted early. Why? Because a secondary deformity due to compression, neck muscle contractures or degenerative changes may result in conditions like cervical myelopathy and neurological decline that contributes to disability, even after reasonable recovery of neck strength. This highlights the importance of attempts to maintain proper neck posture during the period of weakness.
- A 2020 study in the European Spine Journal indicates cervical spine involvement (kyphosis) can be supported by only a cervical brace like the Headmaster Collar, but where there is significant thoracic spine involvement (kyphosis) and global positive imbalance including pelvic imbalance, this requires an additional thoracic support, like the Head Support System.
- A 2021 study in the European Spine Journal found that drop head syndrome can result from degenerative changes in the cervical spine and may also play a role in the onset and progression.
- A 2021 study in the European Journal of Medical Research showed biopsy specimens from the cervical paravertebral region after 3 months identified necrosis, microvessel proliferation, atrophy of the skeletal muscle and ligament degeneration. Persistent skeletal muscle damage of the cervical paravertebral region causes subsequent ligament damage.
Pharmacologic/Surgery
- While treatment of dropped head syndrome is based on an appropriate diagnostic entity, for neuromuscular diseases that are commonly associated like Parkinson’s and myasthenia gravis, there are accepted pharmacologic protocols which should be trialed first, offering the patient an effective alternative to surgery.
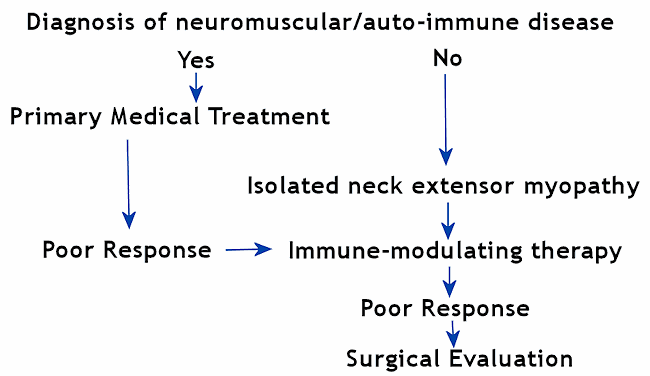
- Patients are often referred to a rheumatologist or neurologist for evaluation of possible autoimmune or neuromuscular causes. If no subsequent diagnosis is made, then the condition is attributed to isolated neck extensor myopathy (INEM) and a course of immune-modulating therapy like corticosteroids may be initiated by a medical internists.
- If a rheumatologic or neurological diagnoses fails to respond to appropriate primary treatment, a course of immune-modulating therapy is often considered as second line treatment.
- If the patient fails to respond to both primary medical treatment and secondary immune-modulating therapy, the patient may consult a spine surgeon for subaxial fusion across the cervicothoracic junction. In the above referenced study, the authors indicated positive clinical outcomes using this method in selected patients.
Fusion from C2 to T2 is promoted to preserve motion in the upper cervical spine, while extending the into the thoracic spine to minimize thoracic kyphosis which moves the center of gravity of the head forward and can contribute to fatigue of the the neck extensor muscles.
The study indicated response to medical and immuno-modulatory therapy treatment in over 70% of patients, and surgery was was an independent predictor of a positive clinical outcome. Fusion across the cervicothoracic junction was a primary factor to success of the surgery and to minimize complications and/or revision surgery resulting from limiting fusion to the cervical spine alone.
- A 2019 study in Neuromuscular Disorders indicated a wide spectrum of both hereditary and acquired myopathies may present with head drop as the predominant clinical feature. In the study, the average presenting age was 68 with 53% achieving a specific diagnosis, with the predominant diagnosis of inflammatory myopathy.
53% of patients responded to treatment and those reporting neck flexion weakness and limb weakness on physical examination were associated with good response to treatment. 89% of patients had abnormal pulmonary function tests, 50% abnormal swallow evaluation, 37% abnormal electrocardiogram and 13% abnormal transthoracic echocardiogram.
Other relevant diagnoses were: myopathy with rimmed vacuoles, radiation-induced myopathy, sporadic late-onset nemaline myopathy, myofibrillar myopathy, facioscapulohumeral dystrophy, inclusion body myositis, mitochondrial myopathy and others. Regarding myopathy associated head drop syndrome, the authors concluded, “Establishing a diagnosis is crucial for timely treatment administration, screening for swallowing and cardiorespiratory involvement, and counseling regarding prognosis.”
- A 2023 study in Medicina (Kaunas) indicates that the level of head drop can lead to horizontal gaze disorder. This can be associated with lower extremity and whole body phase angles (the distribution of water between the intracellular and extracellular spaces).
This is related to cellular composition and measured by bioelectrical impedance analysis. This is associated with physical status according to severity of horizontal gaze disorder. A lowering can be associated with loss of muscle tissue, increase in fluid, and fat. This stresses the importance of correction by appropriate methods.
Case Studies in Dropped Head Syndrome
- A 2020 study in the Journal of Orthopaedic Surgery found that it can be caused by neck injury as well and that those with acute onset dropped head with a history of cervical trauma had a poor recovery rate with conservative treatment (cervical collar, physical therapy, and medication for cervical pain).
The authors did not include those with neuromuscular disease and defined dropped head syndrome as a chin on chest deformity in a natural position with difficulty maintaining a horizontal (forward) gaze in the upright position for even a few minutes, and the deformity was correctable in the supine or back lying position.
They indicated the pathologies of acute (up to 3 months) and chronic onset (greater than 3 months) would be different, with chronic onset more related to degenerative muscle weakness. They concluded, acute onset, balanced global side alignment, and no history of cervical trauma are likely to have a chance to recover by conservative treatment.
- A 2020 case report in the journal Heliyon noted the potential benefit of duloxetine in a patient with drop head, neck pain and gait disturbance with deterioration of condition. There was no neuromuscular or autoimmune diseases. Duloxetine, a serotonin noradrenaline reuptake inhibitor, was given for back pain because nonsteroidal anti-inflammatory drugs were not effective.
Significant improvement was noted after 4 months. Duloxetine is usually prescribed for chronic neuropathic or musculoskeletal pain including depression. The authors indicate a potential disequilibrium of neurotransmitters such as dopamine, serotonin, and noradrenaline in these patients and this drug should be considered as one of the optional treatments. The authors noted 4 other cases that were treated successfully with this method.
- A 2020 case report in the Scandinavian Journal of Rheumatology noted a case of dropped head due to myositis induced by the intravenous cancer drug pembrolizumab. This was noted 2 weeks after the third treatment. The patient had developed myositis and acute rhabdomyolysis, which is a breakdown of muscle affecting the cervical extensors. This muscle breakdown releases myoglobin into the blood, which can cause kidney damage.
- A 2020 case report in Clinical Medical Insights indicates isolated neck extensor myopathy (INEM) resulting from degenerative cervical spondylosis is one of many potential causes of dropped head caused by isolated myopathic changes from chronic injury and overloading of the cervical muscles. This can cause denervation of the cervical extensors.
In this case, manipulative therapy was used in conjunction with an inflatable air pump cervical collar to maintain neck posture and to relieve nerve pressure at home, neck extensor exercises and electrical muscle stimulation. The dropped head state was almost corrected and neck pain was fully resolved near the completion of treatment at 3 months.
- A 2020 Case Reports in Orthopedics noted significant results for dropped head due to cervical spondylosis treated with athletic rehabilitation, where the principle is not just a local treatment but multiple exercises for the whole body. The importance of training for trunk balance/posture control and neuromuscular reeducation is emphasized, as well as pain relief.
- A 2021 issue of Modern Rheumatology Case Reports indicated a case of drop head due to focal myositis that worsened after cellulitis. It was dramatically improved along with the cellulitis treated only with antibiotics. The authors indicate the possibility of preceding trigger event such as infection before making a decision of immunosuppressive therapy to avoid unnecessary increase of glucocorticoid.
With cellulitis, bacteria enter the skin and may spread rapidly. The skin may appear swollen, red painful rash that may be hot and tender with scabs and blisters. One may experience tenderness and a dull achy pain. Without treatment with an antibiotic, cellulitis may be life threatening.
- A 2021 case report in Rinsho Shinkeigaku – Clinical Neurology found an example of drop head in a patient taking oral sitagliptin/Januvia (50 mg/day) for type 2 diabetes, a class of drugs (Dipeptidyl peptidase (DPP)-4 inhibitors). The medication was discontinued and improvement was noted after 1 month.
- A 2021 Journal of Bone and Joint Surgery Case Connect had a 68 year old woman who suffered radiation induced dropped head syndrome and vehemently rejected fusion surgery. A new surgical procedure which avoids fusion was invented and performed called occipitopexy. This is a ligamentous fixation of the occiput (back of the head) to the upper thoracic spine. One year later the patient was very satisfied, able to maintain a horizontal gaze, and rotate her head 20 degrees to each side.
- It is interesting to note that A 2020 study in Expert Opinion on Drug Safety noted rare but adverse drug side effect that may cause dropped head. In their evaluation of the FDA adverse adverse reporting system, the to drug risks were: Pramipexole, ropinirole, levodopa, pregabalin, rotigotine, cisplatin, imatinib and botulinum toxin.
- A 2023 study in Spine Used contrast-enhanced MRI in those with dropped head due isolated neck extensor myopathy (the most common cause) and found intramuscular enhancement of the cervical extensor muscles. There was pronounced involvement of the splenius capitis muscle in all cases. The rhomboid, semispinalis cervici, and levator scapulae were also involved. This method of diagnosis may have implications for rehabilitation.