Neck Related Dizziness: Cervical Vertigo Is The Name For This Symptom
Dizziness is a disturbing symptom and has many possible causes. Many of us have experienced this in one form or another. While it can be related to the neck, there are other causes that require a professional diagnosis in order to rule out any serious issues that require medical attention.
Cervical vertigo can be described as dizziness combined with a neck disorder, where reasonable alternatives have been ruled out.[1] It is a sensation of disorientation in space, which may include an illusion of unsteadiness or motion.

In studies, of 1097 whiplash subjects, 52% of them reported dizziness.[2] Cervical vertigo is also related by individuals with neck problems not related to whiplash, where muscle tenderness and tightness was found in most patients. Facet joint irritation was noted at all cervical levels, cervico-thoracic region was frequently less mobile, and most patients had postural imbalance and poor neck stability.[3]
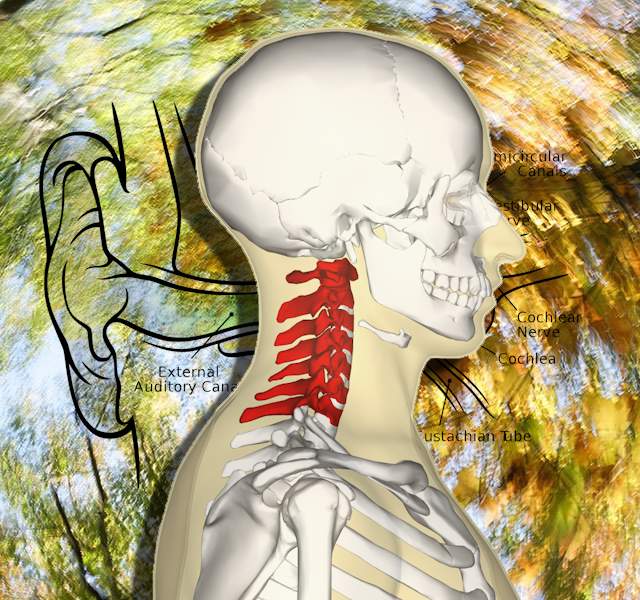
Experimental studies indicate the neck area can induce both nystagmus (involuntary eye movements) and ataxia (impaired balance or coordination).[4] Cervical vertigo may be precipitated by inflammation in the cervical discs and increased muscle tension producing discrepancies between proprioceptive information (position sense) and vestibular system (part of the inner ear) or abnormal sensory stimulation in the cervical spine.[5]
 Neck related cause is a difficult clinical problem where vertigo and neck disorders may overlap with other conditions. Is cervical arthritis causing vertigo or a chance coincidence? Degenerative disc disease is related to dizziness from the neck.[14] Similar symptoms can be associated with migraine headaches, which may also be related to the neck, as well as psychogenic or neurological causes, often called vestibular migraine.
Neck related cause is a difficult clinical problem where vertigo and neck disorders may overlap with other conditions. Is cervical arthritis causing vertigo or a chance coincidence? Degenerative disc disease is related to dizziness from the neck.[14] Similar symptoms can be associated with migraine headaches, which may also be related to the neck, as well as psychogenic or neurological causes, often called vestibular migraine.
Cervicogenic vertigo can be suspect where there is a lack of reasonably related alternatives (brain or cardiovascular disease, ear disease, and migraine). Findings suggest evidence for neck injury: abnormal cervical MRI, stiffness of the neck to palpation, and/or proximity of vertigo to an injury confined to the neck region. Neck pain is highly prevalent and is in about 96% of those diagnosed with cervical vertigo.[2]
Addressing the cervical spine in those with cervicogenic vertigo can be helpful to improved balance, decrease dizziness and neck pain.[6] Medications may help symptoms, but addressing the root cause may prove to be a better solution. Postural education including ergonomics, specific neck exercises, using therapeutic pillows, reversing vertebral compression, and gentle adjustments by a good Chiropractor can help.[15]
This video shows a specific Eye-Head coordination exercise for light headnedness and/or unsteadiness with your neck pain.
Other Common Causes Of Dizziness or Vertigo
In addition to the spinning sensation, you may additionally experience, headaches, nausea, difficulty speaking and walking, sweating, and jerky motions of the eyes. These are disturbing symptoms and your primary health care provider should be consulted.
Benign Paroxysmal Positional Vertigo (BPPV) may be caused by head trauma or aging. It is felt as brief episodes of vertigo associated with changes in head position.[7] Calcium crystals of the inner ear dislodge, entering the semicircular canals which are deeper inside your ear. The misplaced crystals can disrupt the normal fluid movement inside the canals and cause vertigo symptoms.
This can be diagnosed using the Dix-Hallpike Maneuver, where the patient is sitting and then lays back with the head extended about 20 degrees. It is positive if there is vertigo and nystagmus (jerky movements of the eyes) for about 15 seconds as the cause of vertigo.
A re-positioning of the crystals can be done by what is called the Epley maneuver. This is often done by an experienced therapist with the capability to diagnose and correct the problem. The therapist moves your head and neck through a series of quick positional changes using gravity to restore proper crystal positioning.
It has a high recurrence rate and some risk factors for recurrence were noted as cervical spondylosis, long use of computers, hypertension, hyperlipidemia, diabetes, osteopenia/osteoporosis, migraine, female gender, age (≥65years), head trauma, and otitis media.[8] Vitamin D may be considered in those with frequent attacks, especially when serum vitamin D is low.[9]
If you are a hairdresser and notice this in a client when laying them back to wash the hair or do other work, you should let the customer know to consult a health care provider about Benign Paroxysmal Positional Vertigo (BPPV) and how a simple maneuver may help.
Meniere’s Disease:
Your inner ear plays a crucial role in balance and infections as well as other conditions can be the cause of vertigo. Meniere’s disease causes vertigo, ringing in your ears or tinnitus and hearing loss. It mainly affects one ear and may occur at any age, but often starts between young and middle aged.
It is a chronic illness and the severity of symptoms varies. It originates in the inner ear and can be seen in studies as an enlargement of the endolymphatic space called endolymphatic hydrops. It is classified into Certain, Definite, Probable or Possible, based on symptoms and findings.[10]
Conclusion
Vertigo is a common problem and may cause disability and psychological distress. Neck related dizziness is called cervical vertigo, sometimes cervicogenic dizziness, and is a subcategory of vertigo displaying symptoms of sensations of spinning, imbalance or excessive motion, associated with neck pain and stiffness as well as damage in the cervical region due to whiplash trauma.[11]
Disorders of the inner ear are not uncommon and should be ruled out with any other abnormalities prior to the diagnosis of cervicogenic vertigo. Treatments to the neck focused on restoring function and proper spinal alignment like reversing forward head posture may provide relief of symptoms and prevention of reoccurrence.[12,13]
Musculoskeletal pain is prevalent in patients with long lasting dizziness. The strong associations could result in a self-sustaining complex condition. Therefore, in addition to assessing and treating vestibular symptoms, musculoskeletal symptoms and physical health should be addressed.[16]
How Bad Is My Problem? – Take The Quiz
References:
1. Journal of Orthopaedic & Sports Physical Therapy. 2000 Dec;30(12):755-66
2. Laryngoscope Investigative Otolaryngology. 2018 Nov 28;4(1):109-115
3. Disability and Rehabilitation. 2007 Aug 15;29(15):1193-205
4. Annals of Neurology. 1977 Mar;1(3):240-6
5. World Neurosurgery. 2018 Jan;109:347-350
6. Journal of Chiropractic Medicine. 2009 Dec;8(4):156-64
7. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162
8. Ear Nose Throat J. 2020 Aug 10;145561320943362
9. Review J Neurol. 2020 Aug 7. doi: 10.1007/s00415-020-09952-8
10. American Journal of Otolaryngology. 1993 May;14(3):224-9.
11. Am J Otolaryngol. 2021 Jan 12;42(3)
12. European Journal of Physical and Rehabilitation Medicine 2017 Feb;53(1):57-71.
13. Oxford Medical Case Reports. 2019 Dec 9;2019(11):476-478
14. Annals of Medicine 2021 Dec;53(1):639-646
15. Physiother Theory Pract. 2021 Sep 8;1-10
16. Physiother Res Int. 2021 Sep 28;e1923