TMJ Pain Temporomandibular Joint Pain
The temporomandibular joint (TMJ) is the most regularly used joint in the human body. The TMJ, connects the upper and lower jawbones which allows the jaw to open, move back and forth and sideways. It opens and closes about 1500 to 2000 times a day and is also instrumental in several functional movements such as chewing, swallowing, breathing, talking, or yawning. Because the TMJ is a very regularly used joint, its bone, muscle or cartilage may deteriorate over time, leading to TMJ pain or temporomandibular disorders (TMD).
 If you cover your ears with your palms, your thumbs will be on the base of your skull called the occiput. Your palms and fingers will lie across your temporal bones, and the heels of your hands will rest on the angle of your jaw called the mandible. The temporal bone and mandible interact at the temporomandibular joint called the tmj for short. You can locate this joint by lightly placing two fingers directly in front of your ears and open and close your mouth.
If you cover your ears with your palms, your thumbs will be on the base of your skull called the occiput. Your palms and fingers will lie across your temporal bones, and the heels of your hands will rest on the angle of your jaw called the mandible. The temporal bone and mandible interact at the temporomandibular joint called the tmj for short. You can locate this joint by lightly placing two fingers directly in front of your ears and open and close your mouth.
Temporomandibular joint disorders are common in adults; as many as one third of adults report having one or more symptoms, which include jaw or neck pain, headaches, and clicking, popping or grating noises within the joint. The joint has a capsule that contains an articular disc and surrounding muscles have a nerve supply which is thought to be the primary source of pain in TMJ disorders.
The cause of pain, in most cases, is not clear. Some are thought to be joint capsule inflammation or damage and muscle pain or spasm may be caused by abnormal occlusion, teeth grinding (bruxism), teeth clenching, lip biting, stress, anxiety, or abnormalities of the disc in the joint.
Temporomandibular disorder (TMD) is a term that refers to 1 or more conditions that adversely affect the temporomandibular joint or the surrounding masticatory (chewing) musculature. In general, TMD symptoms consist of pain at rest and/or during jaw function, limited range or disturbances of mandibular motion, and noises from within the temporomandibular joint (TMJ). The most common and general categorization of TMD is to separate it into muscle disorders (myofascial disorders that affect the masticatory musculature) or TMJ articular disorders (those that directly affect the TMJ itself like arthritis). It should be noted that both muscle and joint problems can exist at the same time.

TMJ Joint – Joint disorders include arthritis and joint disc displacement.
 |
 |
 |
The TMJ Joint has a disc between the condyle portion of the jaw and where it articulates with the skull which can be displaced and result in clicking or locking.
- A 2021 study in BMC Oral Health found TMJ pain patients were associated with a high rate of condylar erosion (61.3%) on MRI. Condylar erosion occurs in TMJ pain patients with frequencies ranging from 34 to 85%, compared to asymptomatic subjects rates from 0% to 7.4%. Symptomatic TMJ arthritis rates at 94%, compared with asymptomatic TMJs ranging from 6% to 21%.
Condylar erosion is considered an inflammatory subset of osteoarthritis and is considered a sign of progressive arthritic changes potentially contributing to changes in dentofacial morphology or limited mandibular growth.
TMJ Pain & Neck Problems
The temporomandibular joint has been linked to different parts of the body, particularly the neck. Some suggest that posture training may be a positive impact on the muscles because a proper posture can play a relevant role in the relationship between the temporomandibular joint and the rest of the body. It appears that an intimate functional relationship exists between the jaw (mandibular) and the head and neck systems. Patients with temporomandibular disorders often report symptoms of neck pain.
Furthermore, some studies have investigated the relationship between neck symptoms noting that mouth opening is always accompanied by head and neck extension and mouth closing by head and neck flexion. These studies suggest that functional jaw movements use mandibular, head, and neck movements involving the temporomandibular joint, the atlanto-occipital joints between the head and neck, and the lower joints of the neck. The studies have noted the contribution of the upper part of the neck, particularly the atlanto-occipital joint, for proper positioning of the TMJ.
Patients with TMD who hold their heads farther forward relative to the shoulders (forward head posture) have a high probability of experiencing symptom improvement as a result of posture training and being provided with self-management instructions.
Poor head & neck posture is widespread in the general population and appears to be an adaptive, self-perpetuating trait that most people lack the cognitive ability or desire to correct by themselves. Many practitioners have speculated that poor posture may have a negative effect on temporomandibular, or TMD, symptoms and treatment outcome.
Forward head posture is the most common form of poor posture and is assumed by many authors to be related to a multitude of myofascial pain disorders. With this posture, the head’s center of gravity is forward of the spine’s weight-bearing axis, which increases the strain within the posterior cervical muscles, ligaments and joints. Studies have demonstrated that when the head is positioned forward, the upper trapezius muscle activity is significantly higher than it is when the head is in normal alignment and indicates that the patient is more likely have pain from overusing the muscles.
- A 2014 issue of the Journal of Manipulative & Physiological Therapeutics studied posture and tmd pain, finding increased cervical distance or a more forward head posture in those with symptomatic tmj problems compared to those without.
It has been demonstrated that neck muscle activity influences masticatory muscle activity. The additional demand that is placed on the neck by the forward head posture alters the masticatory system so that people are more susceptible to tmj muscle strain, spasm and pain. Posture training usually involves posture exercises performed repetitively to stretch structures that poor posture tends to shorten, strengthen structures that poor posture tends to weaken and create an awareness of the desirable posture.
- A 2008 Journal of the Canadian Dental Association, published the results of a survey that indicated poor posture related to computer use results in chronic jaw muscle pain and other TMD symptoms as well as neck and shoulder pain.
- A 2009 Issue Of Clinics Journal indicated there is an association between posture and tmj pain. They concluded that evaluation of posture is an important aspect of for evaluating and managing temporomandibular disorders.
- The 2014 Issue of the Brazilian Journal of Physical Therapy had an article in which the authors did an extensive research of the literature and found a strong correlation between muscle related jaw pain and the posture of the upper cervical and head region. They also found a moderate correlation between neck posture and joint related tmd.
- A study in the 2003 Journal of Oral Rehabilitation found that patients with tmj muscle pain had significantly more frequent pain in the neck muscles along with more restriction of cervical spine motion than those without tmj symptoms. The authors of the study recommended patients with tmj dysfunction have an examination of the upper cervical area of the neck.
- A 1999 study in the Journal of Oral Rehabilitation found a direct relationship between head posture and movements of the jaw when closing regarding direction and stability of motion.
- A subsequent 2000 study in the Archives of Oralal Biology established a relationship between jaw opening as well as closing with head and neck motion. The authors indicated a functional linkage between the temporomandibular and neck regions, involving the tmj, upper cervical/craniocervical and joints of the cervical spine with coordinated activation of the jaw and neck muscles.
- In a 2008 issue of the journal Cranio (craniomandibular practice), a study used electromyography (emg) to evaluate tmj patients and found an asymmetrical compensation mechanism between the strenocleidomastoid neck muscle and the masseter and temporalis jaw muscles. The compensation was indicated to stability for the head and neck during jaw movements.
- Subsequently, a 2012 issue in the Journal of Manipulative & Physiological Therapeutics used electromyography and found that upper cervical movements have a significant influence on the activity of the masseter muscle of the jaw. The authors provided further evidence for a distinct interaction between the head and upper region of the neck (craniocervical region) and the head and jaw regions (craniomandibular system).
Also, relating to the neck, whiplash injury has also been associated with tmj pain. The mechanism is not clear, however, the 2000 text Dynamic Behavior of the Temporomandibular Joint in 198 Frontiers in Whiplash Trauma, indicates that it is mostly related to the neck. It is stated, “Positioning of a headrest very close to the head would provide a clear means of preventing mouth opening.” The authors indicate that mouth opening is observed during whiplash, but it does not exceed the physiological limits. The authors state “…TMJ dysfunction is more likely due to post-crash neuromuscular changes and/or pain referral of a cervicogenic [neck] nature.”
- A 2015 study in Biomed Research International found a significant correlation between neck and jaw disability. The highest levels of neck and jaw disability were seen with higher levels of muscular tenderness in the upper part of the trapezius muscle and the temporalis muscle. The authors indicate the importance of the neck in treating jaw pain.
- A 2015 study in Cranio: The Journal Of Crainiomandibular Practice found that patients suffering tmj exhibited impairment of upper cervical spine motion, especially those whose pain included headaches.
- A 2020 study in the European Journal of Oral Sciences found that patients with pain related diagnoses are more likely to experience significant upper neck loss of mobility and muscular capabilities than patients with strictly intra-articular (in the joint) diagnoses.
- A 2016 study in Physiology & Behavior used electromyography to study the activity of neck muscles while chewing. The authors detailed normal and abnormal motions and correlations. They found that chewing on one side can affect the opposite side of the neck. This can correlate to neck pain on the opposite side of one sided chewing.
I can personally relate to this as I have been only able to chew on one side for some time due to dental issues that I have been putting off. I have experienced increased neck pain on the opposite side. So, putting off dental work that causes chewing on one side, or tmj treatment with pain one side that leads to chewing on the pain free side, can be directly related to neck pain.
Other TMJ Associations
- A 2007 issue of the Journal of the American Dental Association indicated One out of 3 whiplash trauma sufferers, which often cause neck problems, has a higher risk of having delayed onset TMJ symptoms within a year following the accident. It is well-known that trauma results in injury and pain. Clenching can be considered a form of microtrauma that results in pain. Third molar removal may involve wide opening of the mouth, application of considerable forces to the mandible, and, if performed under general anesthesia, a reduction in a subject’s protective mechanisms. Any of these could result in trauma to the TMJ or the muscles of mastication.
There is also an association to suggest that anxiety, stress, and other emotional disturbances may worsen TMJ disorders, especially in patients who experience chronic pain.
- This has been outlined in a 2015 study in the journal BioMed Research International. The authors indicate that chronic stress may reveal or worsen jaw dysfunction. They indicate increased masseter muscle activity in chronic stress and relate clenching or bruxism as genetically encoded response to stress. Major complaints noted by participants with dysfunction were headaches, pain with wide mouth opening, as well as muscle pain. There is also a high prevalence of tmj disorders among females as compared to males and the relationship is thought to be of a hormonal nature.
- A 2018 review in Neurology Clinical Practice indicates antidepressant associated bruxism may occur, most commonly with fluoxetine (Prozac, Sarafem), sertraline (Zoloft), and venlafaxine (Effexor). Symptoms may begin within 3 to 4 weeks of medication and may resolve in the same period after discontinuation, addition of buspirone, amitriptyline, aripiprazole, chlorpromazine, trazodone, or substitution with another pharmacologic agent.
- A study in a 2011 journal BMC Ear Nose & Throat Disorders, Signs and symptoms of temporomandibular joint disorders related to the degree of mouth opening and hearing loss. TMJ symptoms were more prevalent and problematic for women than men. The more the degree of mouth opening, the more severe the symptoms of pain. Mild levels of pain correlate to normal hearing tests, while more moderate or severe pain symptoms are related to hearing loss.
Grinding of teeth (bruxism), degenerative changes in the joint (ankylosis), joint pain as well as itching of the ear are signs related to TMJ. The study further noted, that movements of the jaw or neck increases pressure on the hair cells in the inner ear which can cause ringing in the ears or tinnitus and vertigo or dizziness; unusual symptoms not often thought to be related to neck pain.
- A 2015 publication in the European Archives of Otorhinolaryngology found there is an increased risk of tinnitus in subjects with tmj disorder. The authors indicated a significant increase in tinnitus symptoms within 3 years of tmd diagnosis.
- A 2019 cross sectional study in PM & R noted the International Classification of Headache Disorders-3 accepted headaches attributed to temporomandibular disorder (TMD) as a valid headache-type. The authors indicted pathways of pain and that migraine, tension-type and secondary cervicogenic headache are often associated with TMD.
- A 2020 study in Laryngoscope found a high prevalence (over 75%) of eustachian tube dysfunction symptoms in temporomandibular joint disorder patients. These symptoms are pressure and/or pain in the ears, clogged or under water feeling, ear symptoms of a cold or sinusitis, ringing in the ears and crackling or popping sounds.
- A 2020 study in the Archives of Oral Biology found genetic associations with joint pain, the temporalis and masseter muscles, showing susceptibility to increased pain sensitivity according to specific genetic factors.
- A 2021 study in Sleep & Breathing defines sleep bruxism as a disorder involving rhythmic (phasic) or non-rhythmic (tonic) masticatory muscle activity during sleep. The results indicated that TMD was diagnosed in 46.4% of those with sleep bruxism, with the most prevalent type being muscular.
- A 2022 study in the Journal of Manual & Manipulative Therapy found the greater the degree of severity of temporomandibular disorders are associated with greater degrees of dizziness, stressing the need to evaluate dizziness with jaw problems.
TMJ Pain From Muscles
Muscular origins show 2 main muscles that can can form areas of strain with referred pain. The “x” shows the area of strain and the red indicates the areas of pain referral. Click on the pictures to make larger.
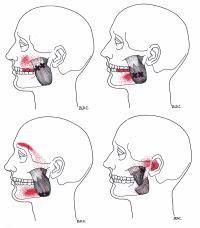 |
 |
| The masseter muscle can have areas of strain that result in restriction of jaw opening (trismus). Tinnitus may be associated with areas of strain in this muscle and is usually one sided. Development of strain in the masseter muscle can be from jaw clenching, sucking the thumb late in childhood, chewing gum habitually, clamping of the jaws on a pipe or cigarette holder, biting off thread by a seamstress, cracking nuts or ice between teeth, poor occlusion of teeth, prolonged dental procedures, emotional tension and referred pain from neck muscle strain of the sternocliedomastoid. | The temporalis muscle can have areas of strain that result in a headache that is felt widely throughout the temple, along the eyebrow, behind the eye and may cause pain in the upper teeth. Development of strain in the temporalis muscle can result from occlusal imbalance, clenching of the teeth, direct trauma from a fall on the head, impact from a golf ball or baseball, or by a car accident, excessive gum chewing, a cold draft over the muscle. Restriction of jaw opening, but not as much as with the masseter. |
- A 2020 study in the journal Pain indicates structural abnormalities in the temporalis muscle related to the volume of the temporalis muscle and its tendon-aponeurosis-complex is found in chronic muscular temporomandibular disorders.
- A 2021 study in the Journal of Headache & Pain indicates that headache attributed to temporomandibular disorder is highly prevalent among patients with chronic myogenous [muscle related] TMD and headaches and often presents as migraines.
- A 2022 study in the Journal of Oral Rehabilitation findings suggest that patients with mucle related pain are more depressed and more anxious than patients with other types of temporomandibular disorder.
Will Correction Poor Vision Hep?
- A 2020 study in Pain Research & Management found that TMJ subjects with vision disorders corrected with standard glasses present EMG values that are significantly higher than those presented by non-TMJ subjects with vision disorders and standard glasses. In fact, in TMD subjects, eye correction did not have a positive effect on the stomatognathic (anatomic system comprising teeth, jaws and associated soft tissues) or pericranial (surrounding the skull) musculature.
TMJ Pain & Jaw Restriction
Determining the level of jaw restriction with TMJ.
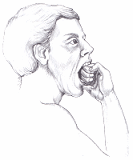 The Three-knuckle Test. The fully opened jaw should admit the first three knuckles of the non-dominate hand in individuals with normal joint and bone structures and without areas of muscles strain. With areas of strain in the masseter muscle, usually only 2 knuckles can be admitted. If there are areas of strain in the temporalis muscle, usually only 2 and a half knuckles can be admitted. Grating or popping sounds during this test may indicate TMJ joint problems and require expert examination.
The Three-knuckle Test. The fully opened jaw should admit the first three knuckles of the non-dominate hand in individuals with normal joint and bone structures and without areas of muscles strain. With areas of strain in the masseter muscle, usually only 2 knuckles can be admitted. If there are areas of strain in the temporalis muscle, usually only 2 and a half knuckles can be admitted. Grating or popping sounds during this test may indicate TMJ joint problems and require expert examination.
- A 2020 study in Cranio indicates joint clicking and correcting deviated mouth opening pattern are signs of early stage disorder, while limited mouth opening and inflammation of the joint are indications of progressive stage and complicated disorder.
Trigeminal Neuralgia
 Sometimes, the symptoms of trigeminal neuralgia can mimic tmj pain. From the picture, you can see the nerve and why symptoms can be similar. Both conditions can cause pain from the muscles of the face and jaw. With trigeminal neuralgia, the pain is usually on one side and is usually described as stabbing, with relief at night. The pain is of short duration and can be minutes or just seconds and there are long periods between symptoms.
Sometimes, the symptoms of trigeminal neuralgia can mimic tmj pain. From the picture, you can see the nerve and why symptoms can be similar. Both conditions can cause pain from the muscles of the face and jaw. With trigeminal neuralgia, the pain is usually on one side and is usually described as stabbing, with relief at night. The pain is of short duration and can be minutes or just seconds and there are long periods between symptoms.
Symptoms of trigeminal neuralgia can include face muscle twitching, redness of the skin and tearing. It is possible that both conditions, trigeminal neuralgia and tmj problems can exist at the same time. Typically, tmj disorders can be on both sides, pain being dull and more constant, problematic at night, short periods between symptoms and no twitching, redness of the skin or tearing.
- A 2020 study in the Journal of Headache & Pain found a significantly increased risk of tinnitus within 1 year of a trigeminal neuralgia diagnosis. The authors indicated further studies should be done to explore the relationship between trigeminal neuralgia and subsequent tinnitus.
TMJ Treatment
- A 2021 study in The Journal of the American Dental Association indicates dental practitioners typically managed the condition using conservative treatments. In this styudy, 82% had pain or stiffness of the jaw on awakening, and 40.3% had low intensity pain. The most frequent diagnoses were myalgia (72.4%) and related headache attributed (51.0%). Self care instruction (89.4%), intraoral appliances (75.4%), and medications (57.6%) were frequently recommended.
Although there is no clear methods of treatment for tmj pain, we next explore methods for TMJ Pain Relief.


