Tinnitus Is Often Described As Ringing In The Ears, But Is A Complex Condition
Tinnitus is a Latin term “tinnire” meaning “to ring”. The actual experience of this sound can vary and have been described as whistling, clicking, humming, hissing and roaring.
What Are The Causes?
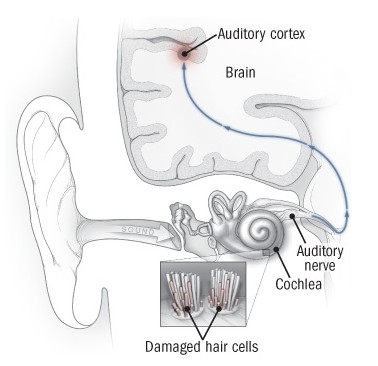
Although tinnitus is common and may not pose a significant problems for most, many will experience it as a life altering and upsetting condition. Most often, it is related to hearing loss associated with ageing, with damage inside the ear and hair cells, frequently with exposure to loud noises. When there is no loss of hearing, tinitus may be located inside the brain, a central cause. An audiogram, which is a common hearing test hearing test will determine if it may be due to hearing loss and is often the first place to start investigation.
 A thorough history and examination by a health care provider is vital, considering possible causes related to cardiovascular, thyroid, tumors and a variety of medications, which include many commonly used pain relievers. Frustratingly, many investigations fail to locate a cause. However, eliminating very concerning causes like tumors is important to relieve some of the stress.
A thorough history and examination by a health care provider is vital, considering possible causes related to cardiovascular, thyroid, tumors and a variety of medications, which include many commonly used pain relievers. Frustratingly, many investigations fail to locate a cause. However, eliminating very concerning causes like tumors is important to relieve some of the stress.
There are many possible causes and this stresses that it is vital to have an evaluation by a health care professional. Factors involved may be loss of hearing, especially high frequency hearing loss, dizziness related to an inner ear disorder, blockage in the ear, hyperacusis – a sensitivity to noise, tumors, inflammation of the ear, sinus problems, headache and vascular disorders, metabolic disorders related to sugar like diabetes, thyroid or lipids, cervical arthritis, hormonal problems, stressful situations, anxiety, depression, medications that are toxic to the ear (ototoxic), stimulants, epilepsy and other disorders.
- A 2021 study in Science Reports of over 90,000 individuals found genetic risk factors and identified 3 genome wide significant variant associations at the the RCOR1 locus.
Electromagnetic Field Hypersensitivity
- A 2009 study in PLoS One found tinitus was significantly more frequent in the electromagnetic hypersensitive group and were independent risk factors for sleep disturbances. The authors concluded, “Our data indicate that tinnitus is associated with subjective electromagnetic hypersensitivity. An individual vulnerability probably due to an over activated cortical distress network seems to be responsible for, both, electromagnetic hypersensitivity and tinnitus.
- In a 2013 Journal of Clinical Otorhinolaryngology, Head, and Neck Surgery, there are indications that exposure to very low frequency electric and magnetic fields can damage outer hair cells of the ear, and this is possibly a risk factor. An earlier 2013 study in the same journal indicated occupational related high strength very low frequency electric and magnetic fields (VLF EMFs) may be related to an increase incidence due to damage of the outer hair cells for long term exposure.

- In a 2013 Environmental Health Journal, there was a study noting several cordless phone frequencies bands were related to tinnitus. It was noted in a 2009 issue of the journal PLoS ONE, the authors suggested that some tinnitus sufferers may have a hypersensitivity to electromagnetic fields. Reduction of cell phone use may provide relief in some of these people along with cognitive behavioral therapy
- In a 2014 study in Alternative Therapies In Health & Medicine indicated self reported symptoms from exposure to wireless smart meters. Usual symptoms of electromagnetic field hypersensitivity were noted and were indicated to have a significant impact on health. Concerns of hypersensitivity surround electrical devices and wiring, energy efficient lighting, appliances, computers and wireless communication.
Symptoms of this hypersensitivity or long term exposure have been anxiety, tension, bone and joint pain, headaches, dizziness and vertigo, forgetfulness, fatigue, insomnia and sleep disturbances, tearing or eye lacrimation, tinitus and hearing loss. I think that electromagnetic hypersensitivity syndrome is possible. As a sufferer for some years, I can say that it does seem that this sensitivity can affect symptoms, however; when a smart meter was installed, I noticed no difference in related symptoms over the years.
Psychological Conditions
- A 2014 issue of the Neuropsychiatric Disease and Treatment journal indicated. “Stress can be considered as a factor leading to damage and dysfunction of the auditory apparatus.” I personally do see a significant relationship with stress. Couple stress with long hours in poor posture hunched over a computer, and you have factors that combine to increase symptoms. The above study also indicated, “The vulnerability to neurotic disorders and the lack of coping capabilities can play a critical role in the clinical history of patients affected by severe tinnitus.”

- A 2014 edition of the European Archives of Otorhinolaryngoly found a direct correlation between depression, anxiety and stress with duration of tinnitus in their study. Males were more affected by stress and anxiety, while female were more affected by stress.
The authors concluded, “… depression, anxiety and stress should be taken into consideration in the treatment of patients suffering from tinnitus.” I’m getting depressed just writing this. But, what comes first, the chicken or the egg? It should be noted that these psychological symptoms are frequently involved with many chronic pain conditions.
- The 2015 International Journal of Audiology indicates a relationship between severity of tinnitus and anxiety and depression. They note that sufferers are at increased risk of depression and anxiety. The authors conclude that early assessment and intervention to reduce depression and anxiety may have a positive influence regarding some troubling aspects of coping with tinitus.
- A 2015 article in the Journal of Neuroscience indicates that serotonin, a chemical neurotransmitter in the brain, is related to the dorsal cochlear nucleus in the brain, which is a central auditory pathway for initiation of sound localization. Increased activity in this area of the brain may relate to central tinnitus.
Therefore, serotonin, noted to be involved in depression and other psychological issues, may play a role. Increasing serotonin is often done through medication, however, there are natural ways to increase serotonin levels like increased sunlight, possibly psychotherapy and increasing dietary tryptophan levels.
- A 2019 study in the journal Clinical Psychopharmacology & Neuroscience found that the effect of tinnitis on life, stress, and depressive symptoms were significantly associated with tinnitus severity in males, where only depressive symptoms and tinnitus annoyance were associated with severity in females. So, depression is associated with symptom severity in both females and males, but stress was associated with severity only in males.
Is Tinnitus Related To Neck Problems?
It is possible for neck conditions to be a cause of tinitis. Strain of neck muscles, sprain of neck ligaments, whiplash injuries, along with degenerative cervical spine changes can make one more susceptible, aggravate, and may actually cause ear ringing. Motions involving some neck exercises and stretches, wearing a soft neck collar for a short period or a neck traction collar may help to confirm this relationship. Proper posture and ergonomics can help with neck problems, along with and healthy and oxygenating breathing techniques help to alleviate stress and strain on cervical muscles.

Seeing a Chiropractor for an examination can help determine if there are neck issues responsive to adjustment or manipulations, particularly the area of the upper cervical spine and I like a low force technique directed in this area called NUCCA, You can learn more and find a Doctor at National Upper Cervical Chiropractic Association.
- A 2000 study in the International Tinnitus Journal indicates that tinnitus can result from an unstable situation of the cervico-cranial junction, which is the relationship between the base of the skull and the first cervical vertebra or neck bone. There are a bundle of nerves and the brainstem, which extends to this region.
It is often compromised in the typical forward head posture, where this area can be compressed. The sound related to this area of the neck can cause a high pitch whistle. It is known to resolve with surgical correction or stabilization in this area from correcting forward head posture. A disc herniation, injuries to the disc and ligaments or even metastatic diseases down to the third cervical area may cause auditory symptoms, which may also respond to surgical repair.
When there is a problem with the neck, it can cause problems for the nerves and muscles situated by the ears. If you also have stress related to neck problems then it can often make the ringing worse. Arthritis in the neck may cause the blood supply of the inner ear to be constricted and that could be a cause.
- A 2020 study in the International Tinnitus Journal found upper cervical nerves can cause tinnitus which can be reduced by treating cervical spine disorders. The authors found a correlation between arthritis at C3/4 and less hearing at 2 kHz in those who responded to treatment.
- In the 2006 Journal HNO, “Functional disturbances of the cervical spine in tinitus”, “Results of the statistical analysis show that patients with tinnitus have characteristic and specific patterns of abnormalities in the joints and paravertebral muscles. The dominant finding is an overall impairment of cervical spine mobility, to which various factors contribute. These include disturbed function of segmental joints of the head and the cervicothoracic junction as well as muscular imbalances of the shoulder and neck muscles.”
- A 2014 issue of the Pain Physician Journal describes a case study where a subject had been suffering left sided tinnitus for 3 years. He had a negative initial medical work-up and noted slight left sided neck pain. X-rays were taken that showed facet joint hypertrophy on the left side. A procedure was done to block and deaden the nerve at C2/3, and this eliminated the ringing, which was still noted at 1 year follow-up.
- The 2013 issue of the Journal of the American Academy of Audiology did a case study on a patient with tinnitus, focusing on normal neck mobility, mobilization of the joints and tissue massage. After 10 sessions, there was a complete reversal of the symptoms. It was noted that certain motions of the neck done against resistance made the ringing worse, so there were indications that the cervical spine was involved.
- A 2020 study in the International Tinnitus Journal found 26% of patients responded to treatment of the 8th cervical nerve, which is in the lower cervical spine. Those who responded best had hearing loss at 500 Hz.
- A 2015 issue of the journal Otolology & Neurotology studied neck dysfunction in chronic tinitus patients. The authors of the study found that cervical spine dysfunction consisting of motion range, pain producing tests, muscle soreness and weakness, along with functional ability questions were significantly higher in the patients with chronic tinnitus.
- A 2016 article in the journal Frontiers in Psychiatry found a single case where a patient suffering from chronic tinnitus for 20 years experienced within 4 weeks of using a cervical collar. The patient used the collar 20 min for the first time and noticed a slight improvement. After 2 weeks for 15 to 20 minute sessions at approximately 3 times per week, the ringing was significantly improved. After 2 more weeks, it was gone.
The collar should significantly support the neck in an upright position, preventing forward inclination. It is also possible to use cervical traction collars for this purpose. This is just one case, and is the exception rather than the rule.
- A 2021 study in the The International Tinnitus Journal found in patients with tinnitus as chief complaint, 64% also have cervical pain, where patients with cervical pain as the chief complaint, 44% have tinnitus. Both groups of patients displayed a high prevalence of postural instability and dizziness, and degeneration of the intervertebral disc.
- A 2021 study in the The International Tinnitus Journal high loudness can be provoked by cervical disc degeneration at C3 to C6 along with anterior spurring of the vertebrae affecting the sympathetic nervous system, which can cause symptoms like accelerating heart rate, decrease intestinal motility, constrict blood vessels, cause perspiration and raise blood pressure.
Thus, it may be related to or have an association with neck problems. When related to the neck, it is called “cervicogenic somatic tinnitus”. Although adjustments did not help me, it is reasonable to take easy to implement measures such as detailed at Neck Solutions or seek professional help from a Chiropractor as a secondary approach. It should not take long to notice a difference after adjusting the cervical spine. The first approach should be medical to rule out any serious conditions, like an acoustic neuroma.
Somatosensory Tinnitus
As discussed above, symptoms may be related to the neck and this is a specific part of somatosensory tinnitus. Other areas that can be related are the TMJ, head, and shoulders. Typically, the pitch, loudness or location may be modified by somatic (body) movements.
- A consensus for diagnostic criteria published in a 2018 edition of the journal Trends in Hearing found somatosensory diagnosis with modulation of symptoms with voluntary movement of the head, neck, jaw or eyes, or with pressure on trigger points.
The authors further relate somatosensory type if associated with simultaneous neck/jaw pain, preceded by a head or neck trauma, symptoms increase with bad postures. Also if symptoms are accompanied by frequent pain in the cervical spine, head or shoulder girdle, presence of pressure tender myofascial trigger points, suboccipital muscle tension (upper cervical spine), tmj disorders, teeth clenching or bruxism, or dental diseases.
- A 2020 study in the Journal of Clinical Medicine found non-invasive orofacial treatment (therapy and occlusal splints in case of grinding) was able to reduce tinnitus severity in patients with temporomandibular related somatosensory tinnitus.
- A 2020 study in Pain Practice found that a higher baseline handicap score coupled with more pain on pressure of the temporalis muscle correlated with better outcomes in treating somatic tinnitus related to temporomandibular pain. TMJ treatment consisted of manual therapy, exercise and education.
Brain Function
- A 2019 study in Clinical and Experimental Otorhinolaryngology found that the severity score is a potential determinant for the prediction of the mild cognitive impairment, associating an underlying mechanism between cognitive deficit and chronic tinitus in patients 65 and older.
The term “mild” can be a bit misleading in that there is a link between mild cognitive impairment and dementia.
- A 2021 study in Scientific Reports found that pre-existing tinnitus was associated with a 68% increased risk of developing early-onset dementia among young and middle-aged adults. The authors state, “The results call for greater awareness of tinnitus as a potential harbinger of future dementia in this population.”
- A 2020 study in the journal Laryngoscope Investigative Otolaryngology found that functional connectivity of the auditory connections in the brain are reduced in tinnitus patients compared to age matched controls as measured by functional magnetic resonance imaging. They were able to diagnose tinnitus with 86% sensitivity and 74% specificity using this method.
There was a significant correlation between increased tinnitus severity score (30 and greater) and decreased cognitive functions. There are earlier studies indicating cognitive impairments, including attention deficit, memory disorder, and poor learning in patients with chronic tinnitus, and have shown to have negative effects on working memory and selective or executive attention.
- An earlier 2016 study in Brain Research found cognitive changes in tinitus patients that were specifically associated with particular areas of the brain, namely, the hippocampus, anterior cingulate and insula. The study showed multiple factors: loudness, distress and duration to be positively correlated with different cognitive measures.
- A 2019 study in the Brazilian Journal of Otorhinolaryngology found poor performance regarding auditory attention ability, and another 2019 study in European Archives of Oto Rhino Laryngology found disruption of the functioning of auditory working memory.
- A 2020 study in Human Brain Mapping studied patients with acute and chronic symptoms and concluded, “This indicates that the appearance and development of tinnitus is a dynamic process involving aberrant local neural activity and abnormal connectivity in multifunctional brain networks.”
- A 2015 study in Trends in Cognitive Sciences indicates higher cognitive and affective brain systems are centrally involved in both tinnitus and chronic pain with striking parallels.
The authors noted reduced gray matter volume in the medial prefrontal cortex is a signature biomarkers in both conditions. They noted the frontostriatal system (ventromedial prefrontal cortex and nucleus accumbens) involved in chronic pain is modulated by serotonin and dopamine, postulating possible future avenues of treatment.
It is noted that the study was on idiopathic (unknown cause) tinitus and the relation to chronic pain was centralized pain, where there is no known cause or no objective pain generator related to the pain, where the relationship is between “phantom sound” and “phantom pain”.
- A 2021 study in PLoS One found chronic pain increases the odds of tinnitus greater than 5 minutes by 64%, while odds of at least weekly, highly bothersome tinnitus was 144% higher. The authors indicate the importance of examining for areas of pain to provide a more comprehensive treatment.
- A 2020 study in Scientific Reports tinnitus patients were 1.54 times more likely to develop Alzheimer’s disease and 1.56 times more likely to develop Parkinson’s disease. The study included 12,657 patients and 25,314 controls with almost 10 years follow-up.
- A 2021 study in Frontiers in Neurology found decreased cerebral blood flow in the auditory and prefrontal cortex in chronic tinitus patients. Headache may accelerate blood flow reductions forming a basis for the neurological mechanism in chronic tinnitus with tension-type headache.
Although the emotional and psychological aspects are more well documented, this is a trend in research that shows some disturbing consequences. Future studies will need to elicit more functional information. However, at this point, it is reasonable, for those who are concerned, to focus on a better diet and nootropics regarding this aspect.
- A 2021 review in the American Journal of Audiology indicates that tinitus, along with hyperacusis (sensitivity to sounds) is due to aberrant nerve signaling in a complex network including both auditory and nonauditory structures.
What Helps?
For the affective component of tinnitus related to stress, anxiety and depression, patients may find relief with tricyclics, an older class of antidepressants. Doctors may also prescribe antiseizure drugs, sleeping pills, muscle relaxants, or benzodiazepenes like diazepam (Valium) or clonazepam (Klonopin).
- A 2021 study in the American Journal of Otolaryngology found that fluoxetine (Prozac) and alprazolam (Xanax) both improved symptoms compared to placebo, however, there was no significant benefit combining the drugs.
 Masking the noise is a common approach to lessen the tinnitus. Many people are only bothered by tinnitus when it is quiet like before sleeping. Masking involves using the noise from a fan, humidifier, turning between radio stations and using the noise that is produced or using music or other soothing sounds through headphones or earphones.
Masking the noise is a common approach to lessen the tinnitus. Many people are only bothered by tinnitus when it is quiet like before sleeping. Masking involves using the noise from a fan, humidifier, turning between radio stations and using the noise that is produced or using music or other soothing sounds through headphones or earphones.
People with hearing loss may find a hearing aid helps. Additionally, masking can be incorporated into the hearing aid itself. By boosting lower frequencies in the hearing aid, those with high frequency hearing loss may find relief.
- The 2010 issue of the Journal of Psychosomatic Research. 2010 Mar;68(3):245-51, found that a self-help book, without therapist assistance, may help in alleviating distress associated with tinnitis and can provide inexpensive treatment that is not bound by time or place. They call this bibliotherapy, which is book therapy.
The book they used is Tinnitus: A Self-Management Guide for the Ringing in Your Ears available below.
Tinnitus Retraining Therapy (TRT) uses a combination of ear devices that emit low volume sounds and counseling. This type of therapy may be expensive and take a couple of years as the brain is trained to turn tinnitus into background noise.
 People who suffer are likely to experience depression, anxiety or sleep disorders. Regardless of cause and effect, these symptoms should be addressed. It has been shown that cognitive behavioral therapy (CBT) can help. This therapy focuses on the emotional response and attempts to break patterns of thinking and behavior that contribute to anxiety and depression.
People who suffer are likely to experience depression, anxiety or sleep disorders. Regardless of cause and effect, these symptoms should be addressed. It has been shown that cognitive behavioral therapy (CBT) can help. This therapy focuses on the emotional response and attempts to break patterns of thinking and behavior that contribute to anxiety and depression.
- A 2021 study in the American Journal of Audiology found that seeking support during the pandemic was associated with significantly less tinnitus distress. The most frequently utilized coping resources were contacting friends and family, spending time outdoors, relaxation, and exercise.
- The Cochrane Database of Systematic Reviews 2010 Issue 2 concluded, “We did not find a significant difference in the subjective loudness of tinnitus, or in the associated depression. However we found a significant improvement in the quality of life (decrease of global tinnitus severity) of the participants, thus suggesting that cognitive behavioral therapy has an effect on the qualitative aspects of tinnitus and contributes positively to the management of tinnitus.”
Since early ringing symptoms can be distressful, trying to address it at this point can help prevent it from becoming a chronic problem. Tinnitus-related sleeping disorders, anxiety, as well as life satisfaction are important factors related to problems with chronic tinnitus distress.
- A 2013 study in the International Journal of Clinical and Experimental Medicine found the Heidelberg Model of Music Therapy approach used early can help with prevention of the chronic condition.
Transcranial magnetic stimulation (TMS), which sends an electrical current into the brain has shown some promise along with electrical cortical stimulation (ECS), however, further clinical trial studies are needed. If you are interested in participating in any of these clinical trials, you can follow the link at government approved Clinical Trials for Tinnitus from the U.S National Institutes for Health.
Often related to neck problems, temporomandibular disorders may affect tinnitus and one should avoid clenching and grinding of teeth and use jaw and neck relaxing exercises.
- A 2014 study in the Journal of Prosthetic Dentistry found a correlation between tinitus and temporomandibular disorders. It was found to be 8 times higher in those with temporomandibular disorders. Treatment directed to the jaw helped in almost 50% of individuals.
The ringing is usually one sided and on the same side as the jaw problem, which may be effected by jaw movements. A dental appointment can assess the need for proper bite and/or a bite plate fitting to wear at night and/or therapy directed to the muscles.
- In a 2016 review published in Frontiers in Neuroscience regarding subjective tinnitus, there are positive effects of cervical spine treatment (manipulations, exercises, trigger point treatment) on severity, as well as decreases in severity and intensity after TMJ treatment (splints, occlusal adjustments, jaw exercises).
Evidently, the results would indicate a somatic type rather than pure subjective, a more broad category to include non-somatic causes as well. However, it may indicate that non-somatic tinnitus may be modified by therapies directed at the cervical spine and/or jaw.
- A 2020 study in Biological Trace Element Research indicates that and is related to symptoms with manganese, cadmium, chromium being elevated and selenium being low. Therefore, reduction or supplementation of these elements should be considered as possible therapeutic goals.
Electrical Stimulation
 A 2017 study in BMC Complementary Alternative Medicine found that manual and electroacupunture had a positive effect after treatment. There was significant effect on uncomfortable scores.
A 2017 study in BMC Complementary Alternative Medicine found that manual and electroacupunture had a positive effect after treatment. There was significant effect on uncomfortable scores.
- A 2020 study in Integrative Medical Research studied the effects of manual acupuncture, electroacupuncture, and transcutaneous electrical nerve stimulation and found that elctroacupuncture was effective at reducing handicap score more than other forms. This form is easily done at home with cost effective units. You can click on the small picture to see a larger version of the points stimulated and a unit that you can purchase for home use.
- A 2022 study in American Journal of Otolaryngology found TENS is an effective, reliable, and practical therapy method to reduce annoyance, severity, loudness, and increasing the quality of life.
- A 2020 study in Frontiers in Psychology found using electrical stimulation to the auricular branch of the vagus nerve via an earclip electrode was beneficial for stress related symptoms like sleep disturbances and anxiety.
It is thought that the bioelectrical impulse flow reduced inhibitory regulation of neuronal hyperactivity and gamma-hyperactivity in the central auditory pathway as well as possible effects via reduced neuroinflammation. It is an easy and non-invasive method to obtain beneficial effects. You must experiment with modes of stimulation, including the optimal stimulation site and parameters, as these have not been optimally defined.
- A 2021 study in Auris Nasus Larynx reviews dietary changes that may help. This includes low sodium, reduced daily alcohol and caffeine, a gluten-free diet, and avoiding specially processed grains.
Drugs To Avoid – If you can
While there are a number of drugs that can cause tinnitus, some of the more common are analgesics like aspirin and NSAIDs (anti-inflammatories like Ibuprofen).
- A 2014 article in the journal Hearing Research indicates acetaminophen or paracetamol to be a possible cause. There are antibiotics like gentamycin, erythromycin and vancomycin, which have been known to be causal.
- A 2010 study in the American Journal of Medicine gives us a clue to the type of analgesic and potential for damaging the ear with acetaminophen being the worse, NSAIDs like ibuprofen second and then aspirin. Many of these are from abuse of the drugs or high dosages, however, your doctor may be able to avoid aggravation by choosing alternative medications.
- A 2009 study in Cases Journal found a genetic susceptibility to aspartame toxicity suggesting cessation of its use may prove helpful for some. It has also been recommended that one should give up caffeinated beverages like coffee, tea, soda and foods like chocolate to see if symptoms are relieved.
- An interesting 2019 study in the International Archives of Occupational and Environmental Health found that although solvent exposure was not associated directly with tinitus, solvents with benzene, ethylbenzene, and toluene concentrations were significantly associated with high frequency hearing loss, which has been linked to tinnitus.
- In a 2019 Audiology Research study, There was an association with levothyroxine used in treating thyroid conditions and PPI (Proton Pump Inhibitors) drugs for the treatment of heartburn and acid-related disorders.
- A 2021 study in Health Reports indicates that hypertension is a potentially modifiable risk factor for hearing loss and tinnitus; either the condition or medications to treat the condition.
Are There Natural Supplements To Help?
Magnesium
- A 2011 study in the International Tinnitus Journal found taking 532 mg of magnesium a day for 3 months significantly decreased severity in those patients who had moderate to high levels of handicap related to their tinnitus. This was a phase 2 study, without placebo, to see if this therapy would help at all. The data was analyzed by the Mayo Clinic and the results suggest magnesium may play a role in treatment.
Melatonin
- A nice study in a March 2010 issue of Medical Hypotheses Journal, indicated Melatonin has been proposed as a treatment for tinnitus, especially on the basis of its positive effects on sleep and its vasoactive and antioxidant properties. It explores melatonin use, explaining its effect on central nervous system resulting in a type of protective mechanism. Melatonin was able to significantly decrease the intensity of tinnitus, especially in men with a history of exposure to noise and having severe symptoms.
- This was also noted in the 2014 issue of the Southern Medical Journal, where the authors indicated that melatonin may be a good treatment option for those suffering from tinnitus. They indicated melatonin may protect against ototoxic drugs, noting the antioxidant property, enhanced sleep and possible other action not understood yet. They recommend a daily dose of 1 to 3 mg.
- More geared towards professionals, a 2019 review in the journal Current Drug Targets presents an extensive focus in to the effects of melatonin in alleviation of aspects related to neural plasticity, oxidative/nitrosative stress, apoptotsis and autophagy.
Ginko
- In a 2014 Edition of the Neural Plasticity journal, they studied the protective effects of Ginko biloba extract, indicating the benefit through the action on the auditory brainstem activity. Other studies have been done and indicate Ginko is moderately effective for helping loudness and severity.
Studies with Ginko biloba have been done with a standardized preparation of Ginkgo biloba extract called EGb 761. Since it is classified as a dietary supplement in The U.S., the ones that are most like the EGb 761 extract used in studies are Ginkai, Ginkoba and Ginkgold brands.
Zinc
- A 2015 study in the American Journal of Otolaryngology found a relationship with zinc levels. They observed zinc levels decreasing with age, discovering a “significant correlation” between increased loudness and severity of tinnitus with low zinc levels (hypozincemia).
- An earlier study in the 2003 journal of Otology & Neurotology indicated similar findings, noting 50mg of supplemented zinc per day. The authors indicated “Improvement of tinnitus and even of hearing may increase significantly if zinc is given for 6 months or more”.
- A 2019 study in Biomedical Journal found that 40 mg of elemental zinc per day significantly improved noise induced hearing loss associated tinnitus after 2 months.
B12
- A 2016 pilot study in the journal Noise & Health indicated a role for Vitamin B12. The study showed patients deficient in B12 (cobalamin) that were given intramuscular injections of the vitamin improved significantly in measured scales for symptom severity. The authors suggest suggest evaluating serum Vitamin B12 levels as an indicator for the likelihood of improvement with supplementation. Low B12 levels may be seen in those with a high level of Helicobacter pylori and dietary factors like poor intake of milk products and vegetarianism.
B2, B3, Water & Protein
- A study in the 2018 issue of Clinical and Experimental Otorhinolaryngology tinnitus related data from over 7,000 individuals 40 to 80 years of age indicated lower body mass index, female, older age, and less intake of vitamin B2 were significantly associated with tinnitus. Vitamin B2 intake was significantly less in individuals with tinitis who were ages 51-60 years. Reduced intake of water, vitamin B3 and protein was associated with tinnitus-related annoyance. Annoyance was significantly related to less water intake in ages 45-55 years, and with less vitamin B3 and protein intake in ages 66-80 years.

Coffee
- A 2018 report in the journal Nutrients found that daily coffee drinkers not only had 50 to 70% less hearing loss than occasional coffee consumers, but had a protective effect on tinnitus, and the relationship was dose dependent; the higher frequency of coffee drinking had more of a protective effect. Brewed coffee had more of an effect than canned or instant in those 40 to 64 years age group. These results suggest a protective effect of coffee on hearing loss and tinnitus.
Can Antibiotics Help
We know some antibiotics can make symptoms worse and they should be avoided when possible. However, an antibiotic, D-Cycloserine, typically employed in the treatment of tuberculosis may have a positive effect. We are familiar that, in some cases, antibiotics can help back pain, can antibiotics helps tinnitus?
- While some antibiotics can increase symptoms, a study was done and reported in the 2015 JAMA Otolarygology Head & Neck Surgery journal in which the authors used the antibiotic D-Cycloserine combined with a computer based brain training program. They studied the effects on tinnitus bothersome and cognitive difficulties. The authors concluded, “D-cycloserine and other putative neuroplasticity facilitating agents could be investigated in the future as a strategy to enhance neuroplasticity-based tinnitus treatments”.
Those who suffer from this condition are aware how bothering it can be, however, sophisticated imaging studies indicates that individuals with tinnitus have problems that can be located in the brain related to emotional processing, perception and attention. These cognitive difficulties can result in problems with memory, concentration, anxiety among others.
The results of the study indicates that the antibiotics did not have an effect on bothersomeness of tinnitus, but did have a positive influence on cognitive problems reported by the subjects taking the antibiotics along with the computer based brain training program.
Sound Therapy
Sound therapy is pretty much a blanket term for different types of auditory therapy used to help desensitize and accelerate habituation to tinitus. There are clinics that can specialize in personalizing this type of therapy to be specific for your particular needs.
Some attempts at reproducing sounds may be effective. It may help to listen to this type of sound for 5 minutes with headphones. This is a general example, so it may help or be annoying. Interesting and sometimes alarming example of what a sufferer may experience.
- A 2019 study in the journal Acta Oto-Laryngologica used mixed pure tones sound therapy and found them effective to reduce symptoms and distress compared with a broad band noise control group.
- A 2019 study in the Chinese Journal of Clinical Otorhinolaryngology, Head, & Neck Surgery found that a custom sound therapy was able to reduce the handicap score and can reduce the negative effects produced by tinnitus.
EDMR
Eye movement desensitization and reprocessing (EMDR) is a type of psychotherapy involving stimulation, like movements of the eyes from side to side. It is increasing in popularity as a treatment for broad range of conditions. It has been used since 1989, particularly post-traumatic stress disorder (PTSD).
Recently, scientific evidence is evolving and forms of this therapy have been used to treat tinnitus symptoms from a pathophysiological perspective. This should be done by a trained professional. There are usually 8, 90 minute sessions. There are some videos that claim to do this, but I would be hesitant to concur. more videos on EDMR.
- A 2018 study in the European Journal of Psychotraumatology determined the effectiveness of a trauma focused approach, eye movement desensitization and reprocessing (EMDR), in reducing tinnitus distress in a a multicenter pilot trial.
- A 2019 study in the journal Laryngoscope found Eye movement desensitization and reprocessing (EMDR) significant both statistically and clinically for improvement in tinnitus symptoms. The effect was maintained at 6 months after treatment. This study used tEMDR, a bespoke protocol.
- As of 2019, more trials using EMDR for tinnitus are underway. Studies using this method in combination with other, more conservative therapies will shed further light on this method.
Intratympanic Steroid Therapy
- A 2019 study in the Indian Journal of Otolaryngoly & Head & Neck Surgery found intratympanic steroid injection to be beneficial. After receiving several number of injections, 60% reported complete disappearance, 25% had residual less severe symptoms and 15% reported no improvement.
- A 2020 study in the American Journal of Otolaryngology found intratympanic steroid therapy showed 80% had improvement from symptoms with 20% showing no improvement.
Do You Experience Tinnitus In Your Dreams?
- In the 2014 journal of Neural Plasticity, a study indicated tinnitus is not experienced when dreaming. They investigated 78 patients at a specialized research clinic, of which 97% did not experience tinitus in their dreams. They hypothesized that during dreaming, a prediction error from interacting with the environment in tinnitus is not present.
The authors note that tinnitus is a “phantom perception”, awareness of sound in the absence of an external source, noting the sound can be “pulled from memory”. It was interesting to note that among individuals with normal hearing, 80% hear “phantom sounds” in a soundproof room. The study has benefits for future research into the nervous pathway and disrupting the pathway to alleviate the symptom. The authors concluded that the perception is “switched off” when dreaming, despite there being awareness, similar to wakefulness.
More Information
There is a main nerve that connects the inner ear to the part of the brain called the auditory cortex. This is the 8th cranial nerve and this technique helps to re-set the nerve and can have remarkable effects. It does not work for everyone since there are many causes, however, the results for many can be very helpful. It is easy to do and requires nothing to buy.
It’s important to know that you are not alone. A great source for information and to find support groups in your area is the American Tinnitus Association (ATA), and I highly recommend it for anyone who sufferers from or cares for someone who is suffering. I found William Shatner’s video from the ATA to be very reassuring. You are not alone, ringing in the ears reduces quality of life for 250 million people worldwide. There is an online test you can take to determine the effects that it has on the quality of your life called the Tinnitus Handicap Inventory. It is also a means to monitor the progression and the effects of therapy measures.
To summarize; there is no cure, however, you don’t “have to live with it”. There are methods to control and relieve symptoms, mainly through medication, therapies and instrumentation. New methods are constantly being studied and hope for better treatments in the future should be on the horizon as more information is discovered.
- A 2020 study in Neuro Endocrinology Letters found tinnitus patients showed higher levels of increased platelet activity, which may play an important role in the development of tinnitus. Increased platelet reactivity can be caused by hyperglycemia, hyperlipidemia, insulin resistance, insulin deficiency and associated conditions like oxidative stress, inflammation, and endothelial dysfunction.
- A 2021 study indicates that total cholesterol, triglycerides and low-density lipoprotein were significantly higher in tinnitus, increasing the potential role of hyperlipidemia associated with altered lipid metabolism in management.
Doctors – or Patients Note
How frustrating that so many conditions I write about here at NeckSolutions, I suffer from. I hope this can bring an interesting combination of perspectives, however, I am human. In my case, I have been suffering from tinitus for a number of years. Beyond the initial panic, which was very troubling; seemingly out of nowhere, I developed symptoms which were quite severe. It was devastating! I desperately tried everything with no results. I spent years trying to find a correlation between anything and my symptoms. Every time I thought I might be onto something….. nothing. Well, the panic and anxiety make it worse. Lack of sleep, which can be a problem with sufferers, makes it worse.
Well, now I am a primary health care doctor, so lets see my own primary doctor and get to an EENT for an evaluation. Is something horribly wrong? Initial medication was helpful in reducing anxiety and getting more rest. My EENT, was Doctor Avraham Hampel. Now, I have studied and corresponded with some of the brightest minds across the globe and am blown away with the dedication, courage and intelligence of some of these individuals.
Doctor Hampel was old school, with many years experience and wonderfully skilled. His personality was amazing and I found an instant feeling of trust and confidence. The type of doctor I always wanted to be. He was able to calm me down, determine I had high frequency hearing loss, the most likely cause, and made sure my ears were healthy. He confirmed my primary doctor’s method of approach, which was minimalistic. This has gone a long way to helping me deal with my tinnitus and I have noticed a decrease in intensity and anxiety, in general, over the years. Dr. Hampel is no longer with us and I sure do miss him.
So, don’t handle this by yourself. Get evaluated and institute some reasonable approaches as discussed above. I know that just saying, try to calm down and it will get better over time seems ridiculous if you are just experiencing tinnitus. I have been there. However, the more you know, the less the anxiety; but an evaluation by a professional is very important to rule out any serious causes. Ruling out any serious causes and talking to a professional can be reassuring and calming, being beneficial for symptoms long term.
- A 2019 study in Otology & Neurotology followed over 30,000 patients to determine risk factors for tinnitis. The potential risk factors included diseases of the ear, upper respiratory tract, psychological, nervous system, endocrine, circulatory system, and hemolytic anemias.
The authors found 5 diagnoses with the strongest correlation were regarding the ear: vestibular neuronitis, Menière’s disease, Eustachian salpingitis and obstruction, presbycusis (hearing loss), and otalgia and ear effusion.
- A 2017 study in PLoS One reported a increased risk of approximately 3 times of developing tinnitus with chronic kidney disease. Chronic kidney disease (CKD) is characterized by progressive and irreversible loss of kidney function over the period of months and years and is divided into 5 stages. Many have this and are undiagnosed.
The authors of the study noted, “In addition to hearing loss, other factors such as diabetes, sleep apnea, previous head injuries, history of arthritis and hypertension have been suggested as risk factors”.
- A 2020 review in European Archives of Oto-Rhino-Laryngology also noted the relationship and indicated those with CKD a prone to developing tinnitus among other otorhinolaryngological induced complications.
- A 2020 report in JAMA Otolaryngology–Head & Neck Surgery found a significant heritability profile with multiple significant risk loci and genes in a large scale genome wide association study. The authors indicated, “These findings may guide gene-based diagnostic and therapeutic approaches to this pervasive disorder.”
- Approaching anxiety using some of the “cleaner” medications used to treat anxiety if present can help. A 2015 study in The Journal of Laryngology & Otology indicates that of all the benzodiazepines used in treating tinnitus, Clonazepam is the one with the best evidence, and is not as likely as some of the others like Diazepam (Valium) to be abused due to its longer half life.
Difficulty sleeping can be not only be assisted through medications, but can be helped by listening to music, or in my case, listening to lectures to the point where I just fall asleep. I have tried supplements and cervical adjustments with no results. I have not done TRT or CBT, however, reading about it helped. Protect your ears from loud noises. It can’t hurt to carry a small set of earplugs around – in your pocket, purse, car, just in case.
- The importance of not handling this on your own is further indicated by a 2019 study in the journal Hearing Research found an association between glaucoma and tinnitus. The authors hypothesize a common mechanism to both conditions, possibly vascular dysregulation due to impaired nitric oxide production.
- A 2020 study in BMC Ophthalmology found patients that had early onset
cataracts have an increased risk of developing tinnitus. The authors indicate they should should receive evaluation for early diagnosis and management if any signs develop.
- An interesting 2020 case study report in The Mental Health Clinician indicated a patient previously on a benzodiazepine (clonazepam) developed tinnitus during a gradual dose taper within 7 weeks of gradual dose reduction to 50% of the original dose. Persistence of this symptoms prevented further dose reductions. The authors reviewed available literature identifying several other cases describing development of tinnitus upon discontinuation or tapering of a benzodiazepine.
In conclusion, the authors stated, “In weighing the risks and benefits of chronic benzodiazepine therapy, tinnitus must be considered as a rare but debilitating and long-term risk of benzodiazepine withdrawal. Providers must be prepared to individualize benzodiazepine tapers and be vigilant about emergence of withdrawal symptoms to prevent undue stress in patients.”
This is interesting because one of the treatment methods for tinnitus is the use of benzodiazepines. As in my case, it has helped and has proved the only method of consistent, long term relief. However, the above case notes previous chronic use not related to tinnitus and then subsequent withdrawal as a risk factor for developing the condition.
While no drug has demonstrated long-term reduction that is replicable, or that is approved by the US Food and Drug Administration for treatment, it is reasonable to address associated or comorbid conditions like insomnia and depression. This helps to highlight the complexity of the issue, the severity of dealing with it, the lack of clear understanding, treatments, and the length of this article.
- A 2021 study in the International Tinnitus Journal found 60% of the tinnitus patients met strict diagnostic criteria of insomnia and only 4% were being treated for their insomnia. The authors concluded, “In addition, our data suggests that tinnitus patients with co-morbid insomnia have a more severe form of tinnitus and thus, may need further care and treatment.”
- A 2021 study in the International Journal of Clinical Practice found those with tinnitus and hyperacusis reported the highest tinnitus severity and those with tinnitus and no hearing loss had the lowest tinnitus severity. Younger age and the presence of mental health problems predicted greater symptom severity for all groups
- A 2021 analysis in EClinicalMedicine states the currently recommended management for tinnitus, such as support and psychologic therapies, are relatively time-consuming and expensive. Some new pharmacologic treatments designed are noted. The authors indicate a potential role for treatments with brain-acting effect (amitriptyline, acamprosate, and gabapentin) or anti-inflammation/anti-oxidant effect (intra-tympanic dexamethasone injection plus oral melatonin) as the preferable effective treatments for tinitus without specific or treatable origin.
- A 2022 study in the Journal of Clinical Periodontology indicate that periodontitis is significantly associated with tinnitus.
An interesting note: We had a bad storm and lost power for 2 days. With everything off, I noticed decreasing levels the first day and no symptoms the second day – completely gone! The power came back on the third day and symptoms started and have continued. Now this is completely anecdotal, but no question in my mind regarding the relationship. I have searched, but no studies regarding this other than the above noted electromagnetic sensitivity. It is impossible to go without power and internet so the possible solution, for me, may be futile.

