Chronic Pain & Sleep Quality Are Related, So Don’t Let Insomnia Make Your Pain Worse
 There is a complex relationship between between pain and sleep.
There is a complex relationship between between pain and sleep.
Neck and back pain, when chronic, often pose the risk of depression. Additionally, pain, including headaches and other musculoskeletal disorders, may affect the quality of sleep. Insomnia by itself can cause many problems, however, many people who have a good quality of sleep find that suffering from back and/or neck conditions may decrease their quality of sleep. This further increases the risk of depression and may lead to a decrease in the quality of life, prolong healing and increase symptoms.
Sleep disturbances are common and insomnia is a prevalent sleeping and is frequently seen with health problems like depression and anxiety. Additionally, it is frequently found in those who suffer pain and studies show approximately 50% of back pain sufferers have insomnia symptoms, which may lead to daytime fatigue, mood disturbance and thinking impairments, affecting everyday function and quality of life. This can also be a factor in disability.
Poor sleep quality can increase how pain is perceived, reducing the tolerance for pain. This can cause an increase in the intensity of pain, loss of function during the day and stress
Do You Have Poor Sleep Quality – Take This Questionnaire To Test For Clinical Insomnia
NOTE: This questionnaire is designed to help understand your sleep quality, determining if insomnia is problematic. The questions are meant to reflect a period over the last 2 weeks. This can give you an estimate of how your sleeping quality has changed or how much a new or chronic condition affects your sleep ability in terms of insomnia. It may be necessary, in addition to improving your pain situation, to consult a therapist who specializes in sleep disorders. This may not only increase the quality of life in general, but improve coping with pain conditions and healing. ANSWER FOR A PERIOD OVER THE LAST 2 WEEKS.
After answering ALL of the items click on the ‘Score‘ button. A new window will open with the Score and Interpretation. For educational purposes only.
Pain & Sleep Problems
Sleep latency (problems falling asleep or time to fall asleep) and sleep maintenance (problems staying asleep or time spent asleep) are frequent problems for individuals living with pain. Scientific evidence indicates sleep problems are also related to worsening or exacerbation of chronic pain.
- A 2008 study in the International Journal of Behavioral Medicine indicated that 1 in 15 to 20 new presentations of chronic pain could be linked to sleeping problems.
- The 2014 Journal of Surgical Research published a study on the effects of sleep deprivation in the temporomandibular joint (tmj). Problems with TMJ Dysfunction can be related to neck pain. The results indicated sleep deprivation increases inflammatory chemicals that cause pain (inflammatory cytokines) in the joint. The authors also noted a relationship between sleep deprivation and blood levels of estrogen, as well as increased levels of stress and anxiety.
- The 2014 BMJ Open Journal presented a study of sleep disturbances and the relationship between neck and shoulder pain as well as arm pain. They found that job strain and sleep disturbance predicts having at least one troublesome episode of neck, shoulder and arm pain, indicating that sleep disturbances can be the modifying factor between stress and neck, shoulder and arm pain.
- A 2014 issue of the journal Preventing Chronic Disease noted an association between painful musculoskeletal conditions as well as migraine headache with sleep disorders, especially in women. The authors suggest treatment for sleep disorders in those who suffer chronic musculoskeletal pain in addition to conventional treatments.
- The 2010 issue of the journal Headache noted high levels of sleep disorders in those suffering from chronic headaches. They exhibited high levels of insomnia, sleepiness during the day as well as problems with snoring. The authors indicate insomnia to be a risk factor for headaches turning into a chronic problem.
- A study of 422 individuals in the 2014 Clinical Journal of Pain, found neck pain patients were less likely to improve if the also suffered from poor sleep quality.
- A 2015 analysis in the European Spine Journal indicated Patients with neck and/or back pain of a non-specific nature are more likely to experience meaningful benefits in disability and pain levels when sleep quality was good, compared to those with impaired sleeping
- A 2020 study in the International Journal of Environmental Research and Public Health compared sleep quality in 1995 health care workers from 389 departments at 19 hospitals. The authors concluded, “In conclusion, poor sleep constitutes a potent risk factor for LBP [Low Back Pain] among healthcare workers.”
- A 2020 systematically review and meta-analysis in Nuerophyschiatrie concluded “Sleep disturbance is associated with risk of back pain. Improving sleep can be a deterrent against back pain. Therefore, interventions to reduce sleep disturbances can help to improve health. On the other hand, the relationship between sleep disturbances and back pain can be two-sided, and back pain can also lead to sleep disturbances.”
- A 2020 study in Psychiatry Quarterly found a correlation between tinnitus severity and sleep quality before the onset of tinnitus, indicating that the sleep quality of the past may have an impact on the development of tinnitus.
- A 2020 study in the Journal of Clinical Sleep Medicine found that greater sleep efficiency may be associated with better reasoning and working memory in those with higher levels of pain, while lower total sleeping time may be associated with better reasoning in those with lowest pain in sedentary middle-aged and older adults.
- A 2021 study in the European Journal of Pain indicates poor sleep quality is associated with seeking medical care for back pain in the long term. The authors recommend early screening for signs of poor sleep quality and referral to interventions for improving sleep quality or reducing pain in sleep to improve pain management.
- A 2022 study in the Journal of Sleep Research found that patients with chronic neck pain have poor sleep quality and poor sleep is at least a correlate of and may be an amplifier of perceived pain.
- A 2023 study in Sleep Medicine found even in acute musculoskeletal injuries, loss of sleep increases pain sensitivity in a possible causative role of the lack of sleep on complex pain states after injuries.
There is support for a range of practical methods to assist with insomnia that can be incorporated into programs that manage pain.
Help For Insomnia
If you have taken the insomnia questionnaire and are indicated to have clinical insomnia, you should seek professional help, especially if reasonable self help methods fail and you get results indicating clinical insomnia consistently.
Tips To Help Insomnia For Pain and Sleep
Try to keep the bedroom cool, quiet and dark. Use a sleep mask or dark curtains to deal with a bedroom that is too light. Try ear plugs or soothing background sounds/music to help with outside noises and keep a window open or use a fan – not directly over the neck to keep things cooler if you don’t have air conditioning on warm evenings.
Try to maintain a regular schedule of sleep. This helps restructure the rhythm your biological clock that can easily get out of whack. Go to bed and get up at the same time, regardless of the day or level of tiredness.
Try to not take naps. Taking daily naps may affect your ability to fall asleep at night. If you must, take a power nap – about 15 minutes and before late afternoon.
Wind down before going to sleep. Refrain from stimulating and/or stressful activities before bed, like exercising, arguing, computers and television. Perhaps substitute these with reading, listening to music or knitting with soft lighting.
Limiting amounts of nicotine, alcohol and caffeine may help. Try to stop consuming caffeine 8 hours prior to going to bed. Alcohol, while it may make you feel sleepy, can decrease the quality of sleep. Nicotine is a stimulant, so minimize this as much as possible.
Control lighting. Melatonin is a hormone produced by the brain that regulates sleep and responds to light. Try getting more natural light during the day. Open curtains or blinds and take outside breaks when possible. At night, use low watt bulbs and try to minimize exposure to artificial lights light computer screens and televisions before bed.
Get out of bed. If you are having troubles sleeping, don’t lay there and think about it, this will increase anxiety, decreasing your chances of falling asleep. Instead of forcing it, get out of bed, read or drink some warm milk or caffeine free tea, listen to some soothing music or take a hot bath. Go back to bed when you are relaxed. Use some methods of relaxation, like deep breathing and/or meditation.
Supplements will not work for everyone, and you need to make sure they will not interfere with any medications you take. Common supplements and herb related methods are herbal teas like chamomile or lemon balm, valerian in capsules or teas and melatonin supplements.
Sleeping aids available over the counter often contain antihistamines, which are usually for allergies or colds. These should be used only short term for insomnia, because studies are lacking and they could promote dependency.
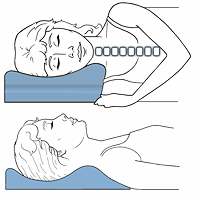
If you have troubles getting comfortable, and well positioned body pillows can help ease postural stress that results in muscle stiffness and joint irritation, making your sleeping experience more comfortable, relaxing, and less painful.
If the above methods fail to achieve reasonable results, talk to your doctor about any prescription sleeping medications. You can explain some of the self help methods you have tried and the test here indicting consistent clinical insomnia findings.
- A 2018 study in Psychiatry Research found higher levels of TV viewing or sitting is associated with sleep difficulties, regardless of physical activity levels, in over 100,000 participants 11 to 18 year old.
- A 2021 study in the Spine Journal found persistent sleep disturbance after spine surgery is significantly associated with failure to achieve meaningful improvements in pain and health related quality of life. The authors concluded, “These results highlight the importance of addressing patients’ sleep disturbance both before and after surgery.”
- A 2022 study in Sleep Medicine Reviews found sleep efficiency and wake time after sleep onset were associated with objective measures of posture and gait.

 Cervical Pillows
Cervical Pillows New Mattresses
New Mattresses Relief Supplements
Relief Supplements