Neck Pain Management
Chronic neck pain in the general population with or without sprain or injury is common. Annual estimates of the prevalence of neck pain among adults ranges from 12.1% to 71.5% with most estimates showing an annual prevalence of between 30% and 50%. There are various grades of chronic neck pain with 5% of patients suffering with grades III and IV neck pain associated with high pain intensity and disability. This poses a complicated questions in neck pain management
While it is well known that neck pain is a common, human phenomenon, what is not known is whether neck pain is likely to improve, reoccur, persist, or worsen. Most of the evidence indicates that between 50% to 75% of people who initially experience neck pain will also report neck pain one to 5 years later. Furthermore, the evidence also indicates that in adults, recovery from whiplash associated disorder is prolonged, with approximately 50% of those affected reporting neck pain symptoms one year after the injury.
Although less prevalent than low back pain, neck pain is very common and may cause persistent pain and disability. Neck pain may originate from intervertebral discs, facet joints, atlantoaxial and atlanto-occipital joints, ligaments, fascia, muscles, and nerve root dura. Cervical intervertebral discs, facet joints, and nerve root dura have been shown to be capable of transmitting pain in the cervical spine with resulting symptomatic neck pain, upper extremity pain, and headaches.
Disc Related Pathology
Chronic, persistent neck and upper extremity pain and radicular pain may be secondary to disc herniation, discogenic pain, cervical spondylosis, spinal stenosis, or post cervical surgery syndrome resulting in disc related pain with or without radiculitis.
Disc Related Pain
Intervertebral disc related pain can be caused by structural abnormalities, such as disc degeneration or disc herniation; correspondingly, biochemical effects such as inflammation can also be the cause. The incidence of cervical disc herniation, however, is less common than lumbar disc herniations.
The mechanical compression on the nerve root that is being irritated by the herniated disc material is an important factor in the production of neck and upper extremity pain. The mechanical, chemical, and inflammatory components produce ischemic neuropathy due to the alteration of blood flow patterns or defects in the neuronal transport mechanism of the nerve root itself. Radicular pain may occur in the absence of nerve root compression secondary to nucleus pulposus extrusion or inflammatory reaction to the chemicals.
Progressive degeneration of the cervical spine on MRI in over 81% of patients during a 10-year period showed 34% developing symptoms. The cervical intervertebral disc is one of the tissues subject to the early aging process, starting as early as 20 years of age, and is often a source of cervical spinal disorders causing neck pain and related symptoms. Advances in basic research on disc degeneration have revealed its possible mechanism, including a decrease in proteoglycan contents and water concentration, the involvement of inflammatory cytokines such as interleukin-1 (iL-1) and iTNF-a, and some genetic factors.
Radicular Pain
The most common causes of cervical radicular pain or cervical radiculopathy are disc protrusion and cervical spondylosis. Other causes include facet joint pathology; vertebral body pathology; meningeal pathology; and pathology from the involvement of blood vessels, nerve sheaths, and nerves. Multiple studies have shown the unique properties of spinal nerves and inflammatory mechanisms, explaining various mechanisms other than mechanical compression and compression affecting dorsal root ganglion. In fact, herniated cervical intervertebral discs have been shown to produce metalloproteinases, nitric oxide, interleukin-6, and prostaglandin E2. These substances are considered to be potential irritants of spinal nerves or inflammation.
Neck Pain Management – Spondylosis and Radiculopathy
Degenerative changes of the cervical spine reach a prevalence of nearly 95% by age 65. These changes are associated with disc protrusion, neuroforaminal narrowing, and spinal cord contour changes in up to 78% of asymptomatic individuals.
Cervical disc herniation occurs in the younger population with traumatic origin and compresses the nerve roots; whereas, spondylosis is a chronic degenerative condition of the cervical spine associated with the formation of osteophytes and compression of the spinal cord.
In most symptomatic cases, spondylosis is associated with aging and with compression of the spinal cord, producing either central or neuroforaminal stenosis in patients older than 55.
Spondylosis refers to degenerative changes of the spine involving the intervertebral discs, uncovertebral joints of Luschka, facet joints, ligaments, and connective tissue of the cervical vertebrae. Degenerative changes of the cervical spine are seen in approximately 10% of individuals by age 25 and in 95% by age 65. The levels most commonly affected by both disc herniation and chronic spondylosis are C6/C7 followed by C5/C6 as these are the cervical segments where the most extension and flexion occurs and a common focus of chiropractic in neck pain management.
Cervical spondylotic myelopathy refers to clinically evident spinal cord dysfunction with the presence of long-track signs due to compression of the spinal cord. Weakness or stiffness in the legs with unsteady gait, together with weakness or clumsiness in the hands, is pathonomic of cervical spondylotic myelopathy.
The progression of weakness may be gradual in some patients or sudden in others following minor trauma. Some patients may complain of hesitancy on urination, even though loss of sphincter control or urinary incontinence is rare and considered a late sign of myelopathy.
Disc Herniation and Radiculopathy
While the most common cause of cervical radiculopathy in 70% to 75% of cases is foraminal encroachment of the spinal nerve due to a combination of factors, including decreased disc height and degenerative changes of the uncovertebral joints anteriorly and zygapophyseal joints posteriorly, herniation of the nucleus pulposus is responsible for radiculopathy in approximately 20-25% of cases.
Cervical disc herniations occur most often between the C5/6 and C6/7 cervical vertebral bodies. Disc herniations can result from degeneration or are precipitated by traumatic incidents such as lifting, etc. As the disc ages, the disc material loses hydration and the annulus weakens, thus increasing the potential for extrusion and herniation. When the disc material protrudes, it is mostly expelled to the lateral side of the spinal canal because of the posterior longitudinal ligament directly compressing the exiting nerve root, which leads to cytokine release and chemical irritation of the nerve tissue.
Neck Pain Management – Spinal Stenosis
Cervical spinal stenosis is a common disease that results in considerable morbidity and disability. It is a complicating factor in neck pain management. Degenerative change is the most common cause of cervical stenosis and can be due to disc herniation, osteophyte formation, or a combination of both, namely disc-osteophyte complex. Tandem spinal stenosis is a degenerative disease that describes a double stenotic lesion involving the cervical and lumbar spine.
Historically, tandem spinal stenosis accounts for between 5% and 25% of all cases of stenosis. However, cervical spinal stenosis is less common than lumbar spinal stenosis. With increasing age, a large proportion of the population exhibits radiological signs of discopathy or spondylosis, leading to constriction of the spinal canal. Thus, cervical spinal stenosis has been detected in 26% of older asymptomatic individuals.
Cervical spinal stenosis may also cause myelopathy which is broadly defined as a symptomatic dysfunction of the cervical spinal cord caused by compressive etiologies. However, cervical myelopathy can occur because of cord compression resulting from one of several physiological factors including spondylolysis/congenital stenosis, disc herniation, ossification of the posterior longitudinal ligament, hypertrophy of the ligamentum flavum, and degenerative subluxation.
For the past 4 decades, there have been several attempts to correlate the clinical severity of spinal stenosis with the degree of spinal cord compression on MRI. However, no methodology has been validated. MRI measurements of maximum canal compromise, maximum spinal cord compression, and compression ratio are reliable and correlate well with the clinical severity of cervical myelopathy.
Neck Pain Management – Post Surgery Syndrome
Cervical post surgery syndrome represents a cluster of symptoms following cervical spine surgery wherein the expectations of the patient and spine surgeon are not met. Animal models of post lumbar laminectomy syndrome demonstrated paraspinal muscle spasms, tail contractures, pain behaviors, tactile allodynia, epidural and perineural scarring, and nerve root adherence to the underlying disc and pedicle. It also has been postulated that there may be a final common pathway with all the described etiologies, which results in peripheral and central facilitation potentiated by inflammatory and nerve injury mechanisms.
Post operative axial neck pain is a common complication even though neurological recovery after laminoplasty is excellent. Multiple factors, including surgical trauma to the posterior cervical muscles and the period of external immobilization, have been suggested as causative factors for the development of pain, the precise mechanism underlying the development of post operative axial pain remains unclear.
Post operative axial pain is multifactorial in nature with soft tissue injuries, such as those that occur due to intraoperative damage of the posterior extensor musculature, are considered to be a major mechanical factor in the development of post operative axial pain. In addition to muscle damage, nerve tissue injuries sustained during surgery also have been suggested as a causative factor of post operative axial pain, and poses a frustrating aspect of neck pain management.
Neck Pain Management – Diagnosis of Discogenic Pathology
An assessment of differential diagnosis is based on a patient’s history and an extensive physical examination which includes a neurological examination; motor examination; sensory examination; reflex assessment; application of provocative maneuvers, including Spurling’s neck compression test, shoulder abduction test, neck distraction test, Lhermitte sign, Hoffman sign, and Addison’s test.

The distinguishing features of cervical radicular pain and somatic referred pain are illustrated in the table. While pain secondary to either the disc or facet joints is limited to the neck, upper back, and head associated with referred pain into the upper extremity, discogenic pain may present as radicular pain and facet joint pain may present as pain below the elbow with referred pain patterns.
Radicular pain is most likely to travel below the elbow, and somatic referred pain is most often limited to above the elbow, but radicular pain may be restricted to the upper back or shoulder girdle, and somatic pain may radiate below the elbow. Symptoms may be confusing because radicular and somatic pain may coexist.
In contrast to the lumbar spine, paresthesia is considered to be more valid than the distribution of pain. The distribution of altered asensation or paresthesia in the hand is also considered more valid than the distribution of paresthesia in the forearm. In addition, paresthesia, with or without pain, occurs in 90% of patients with surgically proven radiculopathy due to disc prolapse. Approximately 45% of patients are unable to vocalize the paresthesia to a distinct region; and they present with diffuse, nondermatomal symptoms. In general, paresthesia affecting the thumb or index finger is attributed to the C6 dermatome; the middle finger, with or without involvement of the index finger, is assigned to the C7 dermatome; and the little finger is assigned to the C8 dermatome.
Overall a patient’s history may not be reliable in assessing cervical spine pathology in reference to diagnostic procedures and neck pain management. A positive Spurling’s, traction/neck distraction, and Valsalva can be used to establish a diagnosis of cervical radiculopathy. The existing literature appears to indicate high specificity, low sensitivity, and good to fair interexaminer reliability for Spurling neck compression test, the neck distraction test, and should abduction (relief test) when performed as described.
For Hoffman’s sign, the existing literature does not address interexaminer reliability, but appears to indicate fair sensitivity and fair to good specificity. Numbness in the upper limb is a reasonably reliable sign, even though it is not a universal feature in patients with radiculopathy. The prevalence rate of numbness has varied significantly from 24% to 48%, and 60% to as high as 86%. Numbness is most often seen in the C6 and C7 dermatomes, indicating the most frequent involvement of these nerve roots.
In reference to imaging, patients 50 years of age or older, plain spinal radiography together with standard laboratory tests are highly accurate in identifying the underlying systemic disease; however, plain radiography is not a valuable tool for nonspecific neck pain in general medical assessment, however, specific manual chiropractic methods make good use of this method.
| SOMATIC PAIN | RADICULAR PAIN | |
| Causes | Facet joint pain Myofascial syndrome Discogenic pain |
Disc herniation Annular tear Spinal stenosis |
| Symptoms Quality | Deep Aching Poorly localized Neck worse than arm No paresthesia Covers a wide area No radicular or shooting pain |
Sharp Shooting Well localized Arm worse than neck Paresthesia are very reliable Well defined area Radicular distribution |
| Modification | Worse with extension Better with flexion No radicular pattern |
Worse with flexion Better with extension Radicular pattern |
| Radiation | Neck to head, shoulder blades, upper back, radiation below elbow unusual, no radicular pain | Follows nerve root distribution, radiation below elbow common, radicular and shooting pain |
| Signs | ||
| Sensory alterations | Uncommon | Probable |
| Motor changes | Only subjective weakness Atrophy is rare |
Objective weakness Atrophy may be present |
| Reflex changes | None | Commonly expressed but seen occasionally |
Neck Pain Management – Facet Joint Pain
Cervical facet or zygapophysial joints have been shown to be a source of pain in the neck and referred pain in the head and upper extremities. Cervical facet joints are well innervated by the medial branches of the dorsal rami with free and encapsulated nerve endings with nociceptors and mechanoreceptors. Anatomical, biomechanical, and physiological bases have been described for facet joint pain.
Evidence is mounting in favor of mechanical injury as being the initiating factor in cervical facet joint pain. Both mechanical injury and inflammation of the facet joint have been shown to produce persistent pain in otherwise normal rats. In addition, mechanical injury of the facet joint increases cytokines messenger RNA in the dorsal root ganglion and intraarticular injection of an NSAID agent alleviates injury induced pain in the same model, suggesting that inflammation has a role in the pain response after a mechanical joint insult.
It has also been shown that painful cervical facet joint distraction induces an immediate and sustained increase of prostaglandin E2 (PGE2) receptor EP2 expression in the dorsal root ganglion, implicating peripheral inflammation in the initiation and maintenance of facet joint pain. Inflammatory mediators such as cytokines, prostaglandins, and neuropeptides have been shown to increase within the joint and dorsal root ganglion in joint inflammation and arthritis. In particular, prostaglandin E2 (PGE2) has been identified as a key mediator of inflammation-induced behavioral sensitivity and increased neuronal excitability.
Neuronal stress activation is associated with painful facet injury, and that joint loading may directly mediate the behavior of the dorsal root ganglia (DRG) neurons in this class of injury. In vivo studies demonstrate that certain facet joint distractions initiate persistent firing of nociceptive afferents in the facet capsule, and induce persistent mechanical allodynia and spinal glial activation. The frequency of neuronal firing increases in rats with neck pain compared to the non-painful and sham groups, as do the incidence and frequency of spontaneous and after discharge firing.
The proportion of cells in the deep laminae that responded as wide dynamic range neurons also increased in the painful group relative to non-painful or sham groups. Excessive facet capsule stretch, while not producing visible tearing, can produce functional plasticity of dorsal horn neuronal activity. The increase in neuronal firing across a range of stimulus magnitude after injury provides direct evidence of neuronal modulation in the spinal cord following facet joint loading, and suggests that facet joint chronic pain following whiplash injury is driven, at least in part, by central sensitization, which requires a different approach for neck pain management.
There are differences in sensory processing between chronic cervical zygapophysial joint pain patients with and without cervicogenic headaches. The main difference between patients with or without cervicogenic headache was the lateralization of pressure hyperalgesia to the painful side of the head of the headache patients, accompanied by cold as well as warm relative hyperesthesia on the painful side of the head and neck. Neuraxial spread of central sensitization is probably linked to the trigeminal spinal nucleus.
There is continuing discussion on the role of facet joint degeneration in chronic neck pain management as a rationale for treatment. The morphology of lumbar facet joint degeneration showed that the pathological changes attributed to facet joint degeneration were articular cartilage thinning, sclerosis of the subchondral bone, osteophyte formation, and hypertrophy. Morphological changes of cervical facet joints in the elderly indicate the prevalence of cervical facet joint degeneration is probably very high in individuals aged 50 years and more, with a tendency to increase in severity with age.
All levels of the middle and lower cervical spines are affected to almost the same degree, whereas in the lumbar spine, an increase in degeneration towards the lower levels is reported. In most cases, the cartilage in the cervical spine was evenly degenerated all over the joint surface while in the lumbar spine, certain regions were reported to be affected predominantly.
Furthermore, following spinal trauma, pathological lesions may be produced in the facet joints and/or accentuate already existing pathology. Hypertrophic changes of facet joints in the cervical spine also have been described. For image and clinical characteristics of patients with cervical facet hypertrophy and the significance of such characteristics, the hypertrophic change of a facet joint occurrs at the mid-level of the cervical spine, usually unilaterally, more frequent in males and is associated with neck pain.
Stretching the facet joint capsule beyond physiological range could result in an altered axonal morphology that may be related to secondary or delayed axotomy changes similar to those seen in central nervous system injuries where axons are subjected to stretching and shearing. These changes may contribute to neuropathic pain and are potentially related to complications in neck pain management after whiplash events.
Whiplash may also cause increased laxity of the cervical capsular ligament. One interpretation is that capsular ligament injuries, in the form of increased laxity, may be one component perpetuating chronic pain and clinical instability in whiplash patients. In fact, a spectrum of injuries could occur in the zygapophysial joints based on the results of postmortem studies. Multiple lines of evidence, using independent techniques, consistently implicate the cervical zygapophysial joints as a site of injury and source of pain, strongly suggesting that injury to these joints is a common basis for chronic neck pain after whiplash.
Numerous investigations conducted in animals, cadavers, healthy volunteers, and patients have documented lesions of various tissues and most lesions are undetected by imaging techniques. However, for zygapophysial (facet) joints, lesions have been predicted by bioengineering studies and validated through animal studies; for zygapophysial joint pain, a valid diagnostic test and a proven treatment are available. The influence of lower cervical joint pain on a range of motion also has been described. The average range of unilateral rotation to the limited side during a flexion-rotation test (FRT) is significantly reduced in patients with lower cervical facet joint pain.
The differences have been demonstrated in pressure and thermal pain hypersensitivity between patients with acute and chronic neck pain and healthy subjects. Widespread decreased pressure pain thresholds in patients with chronic but not acute, mechanical neck pain as compared with controls were identified. Furthermore, as compared with patients with acute neck pain and controls, patients with chronic neck pain also showed cold pain hypersensitivity. There are different sensitization mechanisms between patients with acute and chronic mechanical insidious neck pain. However, neck muscle strength and its relationship to neck pain have not been widely studied.
Neck Pain Management – Diagnosing Facet Joint Pain
The diagnosis of facet joint pain may not be made based on a radiologic evaluation or clinical assessment with certainty. There is little information on the validity or utility of a self-reported history in evaluating neck pain disorders. While routine clinical physical examination is more effective in ruling out cervical radiculopathy than confirming its presence, its usefulness in non-radicular disorders or facet joint pain is debatable.
Local tenderness is not diagnostic of zygapophysial joint pain in the cervical spine. A manual examination of the cervical spine is not a valid means of diagnosing cervical zygapophysial joint pain. There is, however, some evidence that some features of inspection, range of motion, strength, palpation, and provocation tests, can be useful. Range of motion has been described to be moderately reliable, as it does not seem to matter whether it is assessed by the clinician (assessing active or passive range of motion with or without a device) or self-described by the patient.
There is also some evidence that chronic whiplash associated disorder patients and subjects with neck pain and myalgia have less mobility in the cervical spine compared with controls. Patients with chronic neck pain also may have slightly lower neck muscle strength compared with controls. Even then, a role for therapists has been suggested in the screening of patients suitable for diagnostic cervical facet joint blocks. Utilizing clinical prediction guides may allow practitioners to use the results of a patient’s history, self-report measures, and physical examination toward optimal diagnostic and therapeutic decisions, namely, selecting the patient for cervical diagnostic facet joint blocks.
There is no evidence that common degenerative changes on a cervical MRI are strongly correlated with neck pain symptoms. The evidence illustrates that common degenerative changes are highly prevalent in asymptomatic subjects and are also prevalent with increasing age. Moreover, there is no evidence that common degenerative changes on cervical MRI are associated with pain in patients with suspected cervicogenic headache. Multiple evaluations have been shown to be non-diagnostic for facet joint pain. The utilization of an MRI to evaluate patients with acute unilateral neck pain and restricted motion showed no synovial effusion or inflammation around the joints of the cervical spine, confounding the search for a pain generator in neck pain management.
Single photon emission computerized tomography scan (SPECT) was shown to have increased uptake into the facet joints in only 43% of patients. While there is ample literature addressing low back pain, there is no significant literature for the cervical spine for the diagnosis of facet joint pain by SPECT.
Self assessment questionnaires, however, may have utility in routine clinical practice and research by categorizing patients’ clinical presentation, subjective functional impact of neck pain, and force over time. However, there is no evidence that a self-assessment questionnaire alone can accurately diagnose a structural cause of illness in patients with neck pain. There is evidence that generic questionnaires may be more useful than neck specific questionnaires for comparing individuals with neck pain with other disease groups.
Thus, multiple evaluations may be the basis for a suspicion of, but not diagnosis of, cervical facet joint pain. Consequently, diagnostic cervical facet joint nerve blocks have been described as a rational step in the diagnosis of cervical facet joint pain.

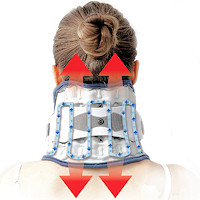 Neck Traction Devices
Neck Traction Devices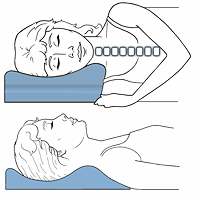 Cervical Pillows
Cervical Pillows Neck Support Collars
Neck Support Collars Ergonomic Aids
Ergonomic Aids New Mattresses
New Mattresses Relief Supplements
Relief Supplements Muscle Therapy Tools
Muscle Therapy Tools Head Supports
Head Supports Topical Pain Relievers
Topical Pain Relievers Special Pillows
Special Pillows Heat Therapy
Heat Therapy Cold Therapy
Cold Therapy TENS Therapy
TENS Therapy Posture Braces
Posture Braces Neck Stabilization
Neck Stabilization