Iliopsoas Muscle Problems Can Mimic Low Back Pain, Hip Pain, And Leg Pain
The psoas (pronounced so-as) syndrome is caused by a problem with the iliopsoas which is comprised of two muscles, the iliacus muscle and the psoas muscle which are joined by the psoas tendon.
Psoas syndrome is a problem with the muscle relating to an imbalance of muscle function. Problems of the muscle occur from strain, spasms, contracture, which is a prolonged spasm and tendonitis, which is inflammation of the tendon that attaches the muscle to bone, and bursitis, which is inflammation of the bura sac that allows smooth motion between the tendon and other structures.
The muscle is comprised of both the major and minor parts, but as the minor is often absent in individuals, this will focus mainly on the major. A better understanding of the role of the muscle and its impact on low back and pelvic stability and may improve suffering from lower back pain.
The iliopsoas is a major flexor of the trunk at the pelvis and is considered the most powerful flexor of the thigh.
Symptoms
There are times when back strain symptoms do not improve in a reasonably short time regardless of treatment and the condition gradually gets worse. The pain seems to spread to surrounding areas in the front of the hip, leg and even mid or upper back areas. It is possible that there is a problem with an iliopsoas muscle spasm or damage leading to a psoas syndrome. It can accompany other conditions affecting the low back and be the main cause of chronic or long standing low back pain.
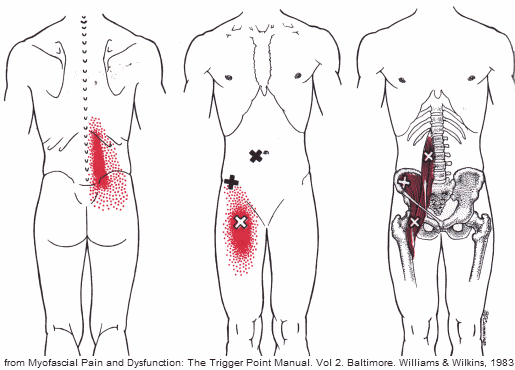
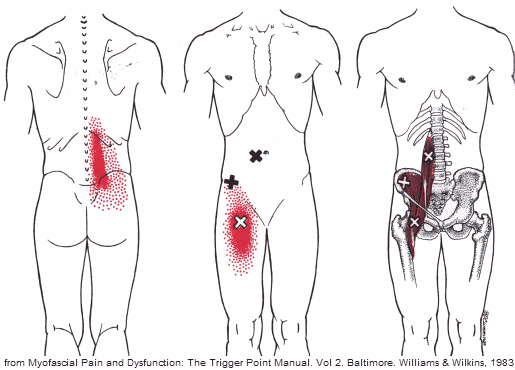
Pain from the muscle will often present as lower back pain and referral areas include the front of the thigh. The psoas can be considered as a pain source in athletes, office workers or anyone who spends much of their day sitting. The syndrome is thought to be prevalent in certain sports including soccer, dance, and hockey.
When the iliopsoas is overworked, or too weak to handle the stress imposed on it, it can go into spasm or tears in the muscle may leave scar tissue causing pain and weakness. This can cause many of the surrounding muscles to compensate and become tight and painful as well. These muscles can pull the spine out of alignment and may lead to disc herniation, usually at the L4-L5 level.
The iliopsoas is a muscle not understood by most people and many doctors and it is difficult for most to describe the pain location any more specifically than the low back. The classic symptoms of spasm or syndrome are lower back pain and the pain may spread to the rest of the back, lower part of the upper back and even into the gluteal area, groin and hip regions.
There may be initial pain upon rising from a seated position. Standing may be painful, but walking and laying down are usually not affected except in more severe or chronic cases. Side sleeping in the fetal position may cause shortening of the muscle and is not recommended. Relief of pain is often experienced by sitting down, although, extending the leg as in driving can make the pain worse. The pain may be worse from long periods of standing and from twisting at the waist without moving the feet.
Strain or spasm of the psoas which leads to chronic dysfunction is the most common reason for the syndrome.
A position which shortens the muscle for long periods can cause spasm. This can happen if you sleep in the fetal position, sit for long periods or when working in a kneeling or crouching position. While a psoas strain (tear) can happen when the muscle is forcefully contracted. This can happen when you run uphill, do a straight leg sit-up or kicking like playing soccer or martial arts.
The pain from a psoas strain can start as a sharp groin pain. This pain may worsen when the hip is flexed or by resisting hip flexion (knee bent with pressure against bringing the leg toward the body). Someone with a psoas syndrome may have what is called an antalgic posture. The typical posture or stance is having pressure on the good side with flexion of the involved side, bent over and foot of the involved side pointed out.
- A 2022 study in the Clinical Journal of Sport Medicine found that increased iliopsoas muscle tightness of the kicking leg in soccer athletes was associated with lumbar stress fracture developing from an imbalance stress reaction of the bone.
Treatment
Treatment of psoas syndrome can be difficult, but usually involves rest, moist heat – shower or tub, and gentle stretching of the muscle to bring it out of spasm. If upright standing is very painful, a degree of mobility can be achieved temporarily by trying to move around on the hands and knees. If there is scar tissue involved, it needs to be addressed and direct access to this muscle is difficult due to the location. The best method of resolving chronic problems with the psoas is using active release technique to improve scar tissue function and strength, although this can be a somewhat painful process – more on this below.
To stretch the right psoas muscle:
1. Lying on your back with a small pillow or cushion under your head, bring your left leg up and clasp it at the knee. Keep your neck relaxed and scapulas anchored.
 2. Breathe in.
2. Breathe in.
3. While breathing out, slowly stretch your right leg out along the floor. It is more important to keep the pelvis stable than to totally straighten the leg.
4. Breathe in.
5. While breathing out, bring your right leg back to the start position.
This stretch gently lengthens the Psoas Muscle to its required length without danger of overstretching, stabilizes the pelvis and helps to avoid low back pain and warms up the psoas in preparation for use.
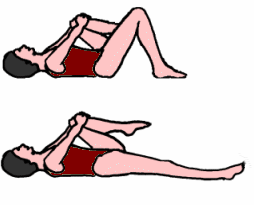
If in acute spasm, you should do nothing more than this next exercise below until the pain begins to dissipate. Do not push yourself and try to relax into the posture. This shows stretching the left muscle.
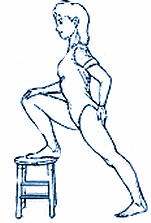 1. Put your right foot on a stool or a stable surface about the same height in a modified forward stance. Hold for a count of 10 to start and gradually increase to tolerance.
1. Put your right foot on a stool or a stable surface about the same height in a modified forward stance. Hold for a count of 10 to start and gradually increase to tolerance.
2. If you are able to do this position without difficulty, slowly bring your arms and hands up towards the ceiling to increase the stretch on your lower back. Hold for an additional count of 10 and gradually increase to tolerance.
Those who have psoas syndrome are likely to have difficulty getting up from a deep-seated chair and are unable to sit-ups. Truck drivers are particularly vulnerable to backache from a psoas syndrome because of the shortened position of the muscle while driving and should routinely perform stretches at every stop on the road. Set the back of the seat to recline some to prevent too much hip flexion. The muscle is also a common cause of back pain during pregnancy. Doing sit-ups can cause problems and it is recommended to do slow sit-backs instead.
After treatment, strengthening is important to help with prevention of psoas syndrome.
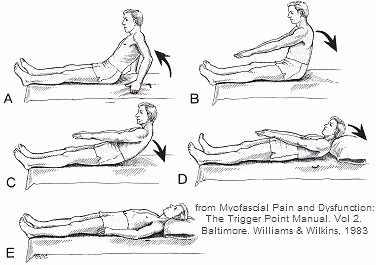 The Slow Sit-Back exercise to improve strength and coordination of the abdominal and iliopsoas muscles as the spine “rolls down”. This exercise requires a less demanding lengthening contraction, rather than the shortening contraction of a sit-up. Three cycles should be performed daily.
The Slow Sit-Back exercise to improve strength and coordination of the abdominal and iliopsoas muscles as the spine “rolls down”. This exercise requires a less demanding lengthening contraction, rather than the shortening contraction of a sit-up. Three cycles should be performed daily.
A. Pushing the body up with the arms from lying back to a seated position.
B. Beginning of the slow sit-back with the lower back flexed.
C. Rolling the back down so each spinal segment reaches the floor in succession.
D. Completion of slow sit-back exercise.
E. Period of full relaxation with abdominal breathing
For sleeping, you can place a pillow or body pillow under the knees when lying on the back. This produces some hip flexion and lessens tension on the muscles to help improve sleep. Again, avoid sleeping in the side in a tight fetal position that shortens the muscle. A sagging mattress can shorten the psoas muscle and cause back pain and morning stiffness. You can place your mattress on the floor or sleep on the floor for a night to see if this helps. If it does, you can get a new mattress or place a half inch plywood under the mattress to help.
The Best Method To Fix A Psoas Syndrome:
This is how I became involved with a particular technique called Active Release many years ago. I had been studying Kung Fu in a closed door school for some time. I developed back pain that was quite severe. I saw all my colleagues, but nothing helped. Finally, I met a Chiropractor who said come in and let me look at you.
From my involvement in martial arts, he suspected the psoas. After a quick muscle test, it was clear to both of us that was the problem. The treatment was somewhat painful, but I had to try something or give up Kung Fu, because I could not kick with my right leg.
After the first treatment, I got up and was astonished, no pain. A few more treatments and that was it. So, I had a lot of scar tissue in the muscle and this technique straightened it out. Needless to say, I took the first seminar I could with the founder of the technique, Dr. Leahy, and had practiced it for years since, with great results for a number of conditions.
There is now a certification system and you can find the nearest practitioner in your location. Highly recommended. From shoulder pain to leg pain, including psoas syndrome, make sure you see a certified practitioner. I have seen therapists that say they know it, but clearly do not.
Video with Dr. Leahy – Soft Tissue Problems & Active Release
It is important, due to all the sensitive structures in the area, to not poke and prod the area on your own. There are structures that can be damaged or it can cause further injury. As you can see from the picture above, nerves run through the muscle. With scar tissue from repetitive or chronic injury, there can be adhesions; where scar tissue adheres to the nerve. As you can imagine, this is painful and needs careful attention to fix. The best method is Active Release and you must see someone who knows what they are doing.
- A 2013 study in the European Spine Journal found that increase muscle size of the psoas in low back pain syndrome indicating increased activity during the instability associated with degenerative disorders of lumbar spine. Reduction in size was seen with marked degeneration of the lumbar spine as well as Modic changes with pain causing a reduction from decreased movement indicting disuse atrophy.
So, for active individuals, especially those involved in sports that stress overuse of the muscle as in skating, swimming, and martial arts (my case), the problem may need active intervention, whereas those who suffer from degeneration and chronic back pain may need more of a strengthening approach. However, if there are intrinsic problems like adhesions, strengthening may be counterproductive.
Seeing a health care professional is recommended. For the muscle syndrome with scar tissue and/or adhesions, Active Release testing results are clear and treatment results are fast.
 The orthopedic differential diagnosis should also include femoroacetabular impingement (FAI) and intra-articular hip pathology. If there is no back pain, it could be gluteal abductor weakness and simple exercises can let you know if this is the cause.
The orthopedic differential diagnosis should also include femoroacetabular impingement (FAI) and intra-articular hip pathology. If there is no back pain, it could be gluteal abductor weakness and simple exercises can let you know if this is the cause.
- According to a 2020 study in the Journal of Pain Research, patients with lower back pain and/or groin pain with tenderness over the iliopsoas tendon attachment to the hip, iliopsoas tendinopathy diagnosis should be considered. CT and MRI are recommended to rule out other diagnoses, including femoral acetabular impingement and osteoarthritis. Ultrasound guided injection of an anesthetic/steroid can be successfully applied therapy and/or diagnosis confirmation.
- A 2016 report in Sports Health indicates an abscess in the muscle is rare cause of hip, low back, or groin pain, but could be suspect with severe groin pain accompanied by fatigue, fevers and nausea. Due to proximity of the muscle with the digestive tract, urinary tract, and iliac lymph nodes, it may be predisposed to contact with infectious material from the surrounding structures and may also spread from distant sites. Severe pain with fever should be considered a medical emergency due to possible abscess.
There are other medical conditions that may refer pain in similar locations. These can be an aneurysm of the abdominal aorta, an abscess in the abdomen, inguinal hernia, cancer of the sigmoid colon or prostate, diverticulitis, appendicitis, Crohn’s disease, ureteral calculi, salpingitis, and prostatitis.
Iliopsoas abscess
Although rare, an iliopsoas abscess can be associated with diabetes mellitus, intravenous drug abuse, AIDS, renal failure, and immunosuppression. Features may be flank/back/abdominal pain, fever, limp, malaise, weight loss, and lump in the groin.

Iliopsoas abscess is the accumulation of suppurative fluid (purulent exudate -pus) within the fascia surrounding the psoas and iliac muscles. Most cases of these abscesses are treated with antibiotics and minimally invasive drainage.
Hip Flexors
The psoas is part of the hip flexors located on the front of the thigh and in the pelvic area and are important to keep the pelvic muscles in balance. The group of muscles are the iliacus, iliopsoas, and rectus femoris – part of your quadriceps that runs from the hip to the knee. Every time a step is taken, the hip flexors are used and sitting for long periods shortens and tightens these muscles.