Fibromyalgia Is A Chronic And Complex Condition With Pain Frequently Involving The Neck And Back
Whereas muscle pain usually involves one or two regions of the body, the pain of fibromyalgia is a syndrome, thus the often used term (FMS) is more widespread with multiple tender points that have a quality different than the neck and back strain patterns we have discussed.
 Women tend to be affected with fibromyalgia more than men, with the onset of symptoms in the 20’s and 30’s. It is often misdiagnosed lending to its chronic nature, unnecessary medical treatment and emotional distress and frustration.
Women tend to be affected with fibromyalgia more than men, with the onset of symptoms in the 20’s and 30’s. It is often misdiagnosed lending to its chronic nature, unnecessary medical treatment and emotional distress and frustration.
Predisposing factors have been postulated to be physical trauma, psychological stress, history of abuse and genetics.
Other chronic conditions are associated with FMS including chronic fatigue, sleep disturbance, myofascial pain, irritable bladder syndrome, irritable bowel syndrome and cognitive dysfunction.
The pain of is often made worse by physical activity, stress, lack of sleep, cold and damp weather. Complaints often found in association are generalized weakness, daily fatigue, muscle and joint stiffness, generalized tenderness, unrefreshed sleep, disturbed mood, anxiety, frequent urination, irritable bowel and multiple chemical sensitivities.
 There are specific tender points associated with fibromyalgia and current diagnosis suggests 11 of these points be present.
There are specific tender points associated with fibromyalgia and current diagnosis suggests 11 of these points be present.
Another clue to diagnosis is painful responses to a stimulus that does not normally elicit pain. For example, a person may perceive light pressure or the movement of clothes over the skin as painful, whereas a healthy individual will not feel pain.
Some conditions which can co-exist or be confused with fibromyalgia are hypothyroidism, myopathy, rheumatic disease, nutrient deficiencies, sleep disorders and mental conditions.
Fibromyalgia patients often forget their appointments and cancel at the first sign of bad weather. Sometimes they get lost on the way, show up for their appointment on the wrong days or at the wrong time. The average patient has seen a dozen or so doctors and have been in chronic pain and distress for an average of seven years. There are numerous complaints including anxiety, pain, depression, fatigue, insomnia, irritable bowel syndrome (IBS), sinus problems, tingling in their arms and legs, night sweats, chemical sensitivities, headaches, reflux, and other symptoms.
How would you feel if you went many nights without sleep, had widespread chronic pain, no energy and no hope! Seeing many doctors, numerous tests, too many drugs which do not help, and continue to get worse, year after year.
Treatments
The list of drugs include anti-inflammatory drugs, antidepressants, anticonvulsant medications, muscle relaxants, tranquilizers and pain medications with poor results and many side effects, many of which contribute to erratic behavior and emotional distress. Side effects from commonly prescribed drugs may cause short term memory loss, fatigue, flu-like symptoms, and depression, morning hangover, mental confusion, lethargy, anxiety and depression, thought disorders and fuzzy thinking and are known to deplete at least one or more essential mood dependent vitamins, minerals, or nutrients such as B6, B12, CoQ10, folic acid, etc.
Pharmacology treatment is complicated and requires close monitoring. Mirogabalin is being tested in phase II trials and is promising with fewer side effects and more effective at a lower dose than pregabalin.
Individuals may also be deficient in the brain chemicals which help regulate mood and mental function. Research shows that the majority of these patients are deficient in serotonin, dopamine, and norepinephrine. These three neurotransmitters are essential for optimal mood and mental function. Serotonin also helps regulate moods, sleep, digestion, bowel movements, pain, and mental clarity. Additionally, individuals with FMS have low levels of the amino acid tryptophan, as well as 5-hydroxytryptophan (5HTP), which are needed for the production of serotonin.
While we still do not know exactly what causes it, we do know that individuals with fibromyalgia have a hormonal imbalance related to the hypothalamus, pituitary and adrenal glands which can create a host of detrimental health conditions.

The main function of the hypothalamus is to maintain the body’s status quo. Because of its wide range of influence, the hypothalamus could be considered the body’s master computer. The hypothalamus receives continuous input about the state of the body and must be able to initiate changes if anything goes wrong. The Hypothalamus regulates blood pressure, digestion (bloating, gas, indigestion, and reflux), sleep/wake cycle, sex drive, body temperature, balance and coordination, heart rate and sweating; all of which can be problematic in sufferers. Studies have shown that over 43% of FMS patients have low thyroid function (hypothyroid) with symptoms of mental fatigue, depression, and poor memory.
Chronic stress may be an underlying factor. Several studies have demonstrated how chronic stress undermines normal hormonal function. Poor sleep, chronic stress, nutritional deficiencies, prescription drugs, and other stressors take their toll when accumulated over a number of years. There are some nutritional supplements that can help restore optimal neurotransmitter levels, especially serotonin and norepinephrine levels, which is a critical factor.
Trials have shown that patients were able to see the benefits from increasing serotonin through 5-hydroxytryptophan (5HTP) replacement therapy which included: decreased pain, improved sleep, fewer tender points, less morning stiffness, less anxiety, improved moods including in those with clinical depression and increased energy. 5HTP also boosts melatonin levels by 200 percent.
Serotonin receptors are more abundant in the intestinal tract than in the brain – one reason people get “butterflies” in their stomach when they get nervous. Serotonin controls the rate at which food moves through the intestinal tract. Irritable bowel symptoms, commonly seen in fibromyalgia, usually disappear quickly once the level of serotonin is raised. If you have irritable bowel syndrome, taking 300mg of 5HTP 100mg three times a day along with a good optimal daily allowance multivitamin with magnesium would be a good supplement to try.
S-adenosyl-L-methionine (SAMe) increases the action of several neurotransmitters, including serotonin, norepinephrine and dopamine and helps keep mitochondrial levels at peak levels, increases brain function, and has potent pain blocking properties. Individuals with FMS have been shown to be deficient in the amino acid methionine, from which SAMe is produced by the brain. Studies involving SAMe have shown dramatic improvements in pain reduction. One study showed that patients taking SAMe for a period of six weeks had an improvement of 40% in pain reduction and 35% improvement in depression.
More than 100 peer reviewed studies show SAMe to be a safe, effective, and fast-acting antidepressant. Furthermore, SAMe has been shown to restore normal hepatic function in the presence of various chronic liver diseases (including alcoholic and non-alcoholic cirrhosis, oestrogen-induced and other forms of cholestasis), to prevent or reverse hepatotoxicity due to several drugs and chemicals such as alcohol, paracetamol (acetaminophen), steroids and lead, in addition to having antidepressant properties.
An amino acid found in green tea (L-theanine) has a calming effect on the brain. The usual dose is 50-100mg taken on an empty stomach, two to three times daily. L-theanine creates a relaxing effect in approximately 30 to 40 minutes after ingestion.
- A 2016 study in the International Journal of Rheumatic Diseases found supplementation of Vitamin D3 for 3 months at 50,000 IU/week provided improvements in musculoskeletal symptoms, level of depression and quality of life of patients with chronic widespread pain and fibromyalgia. This was backed up by a 2022 study in Expert Review of Clinical Pharmacology.
- A 2021 study in Nutrients found of the fibromyalgia patients studied, about 85% used dietary supplements, the most common were vitamin D, magnesium, and omega-3 fatty acids.
If you suffer from FMS, a nutritional supplement regimen of 5HTP and SAMe, along with a good optimal daily allowance multivitamin, fish oil, malic acid, and generous amounts of magnesium may provide a good solution to help reverse the “brain fog,” poor energy, chronic pain, mood disorders, and sleep disturbances so common in fibromyalgia. It may also be necessary to seek chronic pain management methods in coping with neck pain, our article on managing chronic whiplash, and other areas of concern.
- A 2015 systematic search in Clinics & Experimental Rheumatology noted that being overweight and obesity are related to the severity of worsening FMS with higher fatigue, pain, less sleep, and more mood disorders. The authors suggest weight control is an effective tool to improve symptoms. They also noted non-coeliac gluten sensitivity have overlapping symptoms and recommend elimination of gluten from the diet as part of a multidisciplinary treatment.
- A 2022 study in Nutrients found magnesium supplementation daily of 100mg improves mild to moderate stress and reduces the pain experience and could be a useful treatment to improve the burden of this disease.
- A 2022 study in Nutrition Reviews indicates while there is no specific diet therapy for treatment, studies indicated that nutritional supplementation, modified high-antioxidant diets, and weight control are beneficial in alleviating symptoms.
- A 2019 study in the Journal of Alternative & Complementary Medicine compared the effects of 10 sessions of acupuncture to 15 sessions of modalities consisting of hotpacks, transcutaneous electrical nerve stimulation (TENS), and ultrasound to the tender points of the neck and upper back. The other group (n = 22) received 10 sessions of formulated acupuncture aimed at treating pain of the neck, upper, and lower back regions.
The authors found benefit in both groups, but one group was not more beneficial than the other. With the focus on active treatments such as exercise, insurance coverage for passive therapies have reduced. Fortunately, many of these therapies can be used successfully at home and are very reasonable.
- A 2019 study in Rheumatology International found that women with fibromyalgia suffered from poor postural stability and spine posture. The authors suggest optimal treatment should include postural training, stability and trunk position sense.
- A 2020 study in Somatosensory & Motor Research found that placing material with a thickness of 0.8 mm under each great toe caused an improvement of body balance in those with FMS. This is an interesting intervention strategies in the management with those who suffer balance difficulties.
- A 2020 study in the Journal of Back & Musculoskeletal Rehabilitation found that heavy metals like aluminum induce oxidative stress and decrease the levels of essential trace elements such as magnesium and zinc, which may be responsible for severity of symptoms.
Fibromyalgia Related Information
- A 2014 study in Semininars in Arthritis & Rheumatism used functional MRI studies of the brain in fibromyalgia patients and found region specific changes in gray matter volume, decreased connectivity in the descending pain modulating system, and increased activity in the pain matrix associated with central sensitization.
- A 2018 study in Anesthesiology indicates as a result of central sensitization and neuro-inflammation in the spinal cord and brain, which can also cause this sensitization. This type of inflammation causes sustained increase of inflammatory cytokines and chemokines in the central nervous system, promoting widespread pain affecting multiple body sites.
Thus medications that address central sensitization and/or neuro-inflammation may be a focus of attention for pain relief. These include medications like duloxetine and TNF blockers like etanercept and infliximab.
- A 2019 report in Oral Surg Oral Med Oral Pathol Oral Radiol. of an extensive database search found a high occurrence of jaw pain and tmj disorders in FMS patients, prompting the authors of the study to indicate that jaw pain disorders should be considered as part of a strategy to improve pain management.
- A 2019 study in the Journal of Pain used patients suffering from fibromyalgia as a chronic pain population to compare with an acute pain population and the effects on attention, the cognitive symptoms in pain. They found the chronic pain patients were distinctly impaired in performing divided attention tasks.
Divided attention tasks are attention on multiple tasks/ideas at once, or multitasking. Examples are singing with a song when driving, conversing when walking, and listening to music while shopping, as opposed to acute pain, where attention switching tasks were effected. This helps elucidate some cognitive symptoms experienced by FMS patients, but has implications for chronic pain in general, as seen with chronic neck pain and chronic back pain.
- A 2020 study in Advances in Rheumatology found that women with a polymorphism of the serotonin receptor gene HTR2A with a genotype GG had a higher risk of developing fibromyalgia (almost 25%) and that these patients have lower limb muscle strength.
- A 2020 study in the Journal of Back and Musculoskeletal Rehabilitation concluded, “This study showed that the prevalence of sleep and balance disorders is higher in FMS patients. A relationship was reported between the sleep quality and balance and functional status and frequency of falls.
- A 2020 study in Seminars in Arthritis and Rheumatism found chronic pain conditions involving head/jaw pain, IBS (Irritable Bowel Syndrome) and depression were elevated among patients compared to other conditions, while anxiety disorders were less common.
- A 2022 study in the International Journal of Environmental Research and Public Health found that physical activity does not mediate the relationship between fatigue and quality of life. However, fatigue dimensions associated with fibromyalgia had a negative and significant association with physical and mental health indicators.
- A 2023 study in BMC Public Health indicates being overweight/obesity, very low physical activity level, alcohol consumption, and smoking, were associated with an increased risk of reported fibromyalgia.

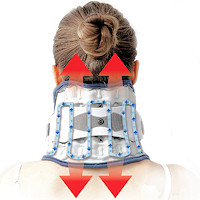 Neck Traction Devices
Neck Traction Devices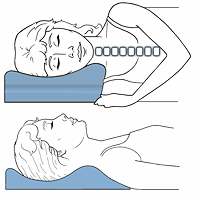 Cervical Pillows
Cervical Pillows Neck Support Collars
Neck Support Collars Muscle Therapy Tools
Muscle Therapy Tools Head Supports
Head Supports Topical Pain Relievers
Topical Pain Relievers Special Pillows
Special Pillows Heat Therapy
Heat Therapy Cold Therapy
Cold Therapy TENS Therapy
TENS Therapy Posture Braces
Posture Braces Neck Stabilization
Neck Stabilization Ergonomic Aids
Ergonomic Aids New Mattresses
New Mattresses Relief Supplements
Relief Supplements