Cervical Angina – Chest Pain Related To The Neck
Cervical angina is chest pain resembling true cardiac angina but originates from the neck disorders. With poorly explained noncardiac related chest pain, this is diagnosed based on negative cardiac workups, positive cervical neurologic examination, and imaging findings of herniated disc, spinal cord compression, or foraminal narrowing or encroachment.
The mechanisms of pain are not clear as there are numerous neurological pathways. Conservative treatments include neck collar, traction, and nonsteroidal anti-inflammatory drugs are usually successful in most patients. If these treatments repeatedly fail, surgery may be indicated to relieve symptoms when a clear pathological generator is related.

According to the New England Journal of Medicine, only 15% to 25% of patients suffering acute chest pain actually have a coronary syndrome. Most patients undergo cardiac rule out procedures and are diagnosed as having noncardiac chest pain. It can be seen with certain gastrointestinal diseases, but can be also caused by musculoskeletal conditions.
According to a clinical trial in the journal Spinal Cord left chest pain was associated with radiculopathy or pinched nerve signs, whereas pain behind the sternum and above the stomach tended to be associated with myelopathy. Some other common signs are neck and arm pain, fatigue, and headache at the back of the head.
According to a 2015 publication in the the journal Neurohospitalist history includes previous cervical radiculopathy, upper extremity weakness or sensory changes, back of the head/occipital headaches, or neck pain. Pain induced by neck motion or movement of the upper extremity. Neck injury or recent manual labor (lifting, pulling or pushing, yard work…) and pain persisting for greater than 30 minutes or less than 5 seconds (although exceptions exist).
Patients with cervical angina often experience anxiety, depression, and disabled daily activities. The pain is often in the front of the chest and is sharp, achy, or crushing. It may be at rest or made worse with neck motion and can be paroxysmal – sudden attack(s) or continuous.
Over half may experience autonomic symptoms such as dyspnea (difficult or labored breathing), nausea, vertigo or dizziness, diplopia (double vision), and other sympathetic nervous signs like rapid heart beat, sweating, agitation and muscle rigidity.
Cardiac workups must be performed in order to rule out true angina. Cervical imaging can be critical in the diagnosis of cervical angina once coronary artery disease has been adequately ruled out. MRI is recommended for functional
assessment and may show degenerative changes, disc herniation, spinal cord compression, or nerve root encroachment. Along with medical history, examination, and radiographic findings, this can support the diagnosis of cervical angina and the real issue dealt with accordingly.
 On a personal note, I experienced this in my early 30’s. I was doing manual labor and suddenly experienced neck, left arm, chest pain, shortness of breath and sweating. It was a bit shocking at first, but I calmed down, however; my wife, who found me on the floor in this condition, insisted I go to the hospital. After ruling out a cardiac issue, my suspicions were later confirmed by MRI – clear herniated disc. Nonetheless, it is quite disturbing not only for the one experiencing it, but for others witnessing it.
On a personal note, I experienced this in my early 30’s. I was doing manual labor and suddenly experienced neck, left arm, chest pain, shortness of breath and sweating. It was a bit shocking at first, but I calmed down, however; my wife, who found me on the floor in this condition, insisted I go to the hospital. After ruling out a cardiac issue, my suspicions were later confirmed by MRI – clear herniated disc. Nonetheless, it is quite disturbing not only for the one experiencing it, but for others witnessing it.
The herniated disc was classic and I used conservative treatment methods and it basically resolved after about 3 months. However, my neck was never quite the same after that. The initial herniation was very painful and the cascading of inflammatory mediators caused the symptomatic presentation which included cervical angina, the primary symptom. Although I did suspect a herniated disc, the presentation of symptoms startled me, but mostly my wife.
It was good to rule out a cardiac event which especially put my wife at ease. She drove me to the hospital, but you should not hesitate to rule out something that could ultimately be life saving instead of trying to be a stupid hero like me who just wanted to lay there until it stopped.

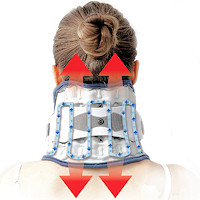 Neck Traction Devices
Neck Traction Devices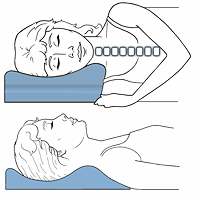 Cervical Pillows
Cervical Pillows Neck Support Collars
Neck Support Collars