Neck Related Sleep Apnea
Sleep apnea has many causes and there can be many factors involved. Because the neck and cervical spine is very close to the upper airway, symptoms can be produced by neck problems in certain individuals.
The condition has a significant impact, not only on sleep, but in quality of life, daily activities, and contributes to higher health care costs. A comparative Study in the journal Sleep indicates and in the general adult population, 80% to 90% of those with this condition are untreated and undiagnosed.
It is a chronic condition with partial collapse or anatomical obstruction of the upper airway during sleep. Due to inadequate quality and/or quantity of sleep, sufferers often exhibit related problems during the day, like excessive daytime sleepiness and poor cognitive function. Some of the more serious consequences can be secondary cardiovascular disorders.
While central apnea is caused by dysregulation of the respiratory center, obstructive apnea is caused by narrowing of the upper airway. Most cases are obstructive, followed by mixed, then central. Doctors measure severity by the AHI (anea–hypopnea index, which measures the number of disturbances per hour of sleep: 5 – 15 per hour, mild; 15 – 30 per hour, moderate; and greater than 30 per hour, severe.
With obstructive sleep apnea, the normal cartilage and bone structures surrounding airway become compromised. Factors like obesity, abnormalities of the jaw of face, and airway tissue abnormalities can predispose apneic events.
Is Your Neck An Indicator Of Obstructive Sleep Apnea?
- A 2015 study in the North American Journal of Medical Sciences proposed a simple and accurate diagnostic test. The authors indicate neck circumference is associated with obstructive apnea and used a grasp test for identification.

The results indicated a positive test called Easy Sleep Apnea Predictor (ESAP) (inability to span the neck) was 100% predictive of the condition in a general sleep clinic population.
The Neck Connection
- A 2020 review in the Sleep Medicine journal found that cervical spine lesions, fusions, and abnormalities can reduce the retropharyngeal space and are associated with obstructibe apnea, likely due to worsening posture and decreasing range of motion.
- A 2010 literature summary in the International Journal of Dentistry found a developmental correlation between cervical spine fusion and developmental craniofacial morphology. Typically described was a backward inclination of the upper cervical column with a exaggerated cervical lordosis – this configuration is similar to the compound angulation seen with forward head posture.

Structures of the neck have been demonstrated to affect patency of the upper airway. Fusions, osteophytes from degenerative arthritis and rheumatoid arthritis, along with more rare pathologies like osteochondromas are suspect. Poor alignment between the bottom of the skull and the first cervical vertebra called the Atlas may predispose patients to apnea, both prior to and after fusion surgery.
As a Chiropractor, the relationship between the skull and the first cervical vertebra has been an area of focus since the founding of the profession. The specific area relates to the brain stem which regulates life sustaining functions like breathing, heart rate and swallowing. This area helps transfer messages to and from the brain and spinal cord.
There are specialties of Chiropractors that focus on the upper cervical region. One is NUCCA (National Upper Cervical Chiropractic Association) and another is a method I used called Grostic Technique. Both use low force safe technique and in depth analysis.
- A 2014 literature review in the European Spine Journal elucidates the relationship between apnea when sleeping and cervical spine pathology. Altered craniovertebral angles, as seen in the upper cervical spine, can reduce the retropharyngeal space, increasing the risk for compromise of the upper airway, especially during flexion of the neck, causing symptoms of apnea during sleep.
In the above study, the authors concluded, “In addition, occipital–cervical alignment may be a factor. It is important for the clinician to be aware of the role of the cervical spine in producing symptoms of OSA [obstructive apnea] in certain patients. Further research is needed to elucidate the association between cervical spine anomalies and sleep apnea.”

- Interestingly, a 2011 study in the Clinical Journal of Pain documents the role of temporomandibular joint disorders in obstructive apnea. This disorder also has relationships between the jaw and neck, and is affected by head/neck postural alterations and muscle dysfunctions.
Positional Therapy & Sleep Apnea
- In the 2014 Journal of Sleep Research, the authors ask the questions, “Are we missing a simple treatment for most adult sleep apnea patients?” Indicating obstuctive apnea can be divided into positional and non-positional individuals. Positional individuals have most breathing problems sleeping on the back. By simply sleeping on the side, symptoms of apnea may be reduced or even eliminated.
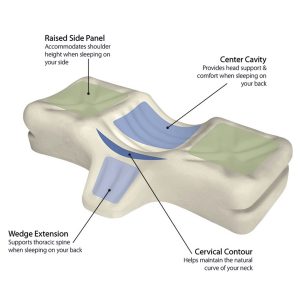
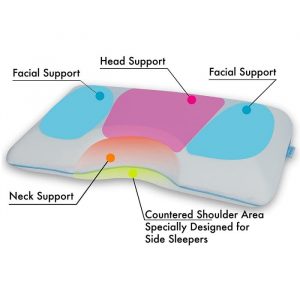
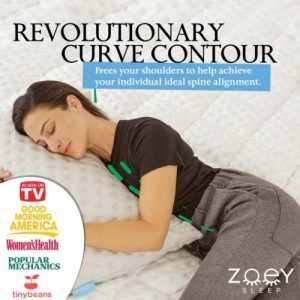
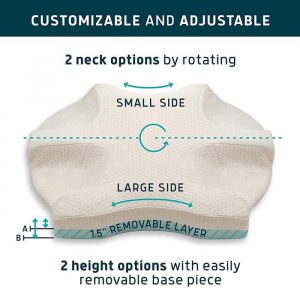
The authors recommend positional therapy by avoiding back sleeping as a valuable therapy for mild to moderate obstructive apnea, indicating they represent between 65 and 87% of obstructive apnea patients, and this would be a “… cheap and effective solution for them.” For those with neck problems, there are special side sleeping pillows and “anti-snore pillows” that can help.
- A 2021 study in the Journal of Sleep Research found that when back sleeping, head flexion (bent down) was associated with more obstruction, whereas head rotation improved obstruction. For back sleepers, it is important to have a pillow that supports the natural cervical curve. Head rotation better approximates side sleeping, which is the best position.
This is why, although results will vary, special pillows are very popular positional therapy devices.
- A 2021 study in the journal Sleep & Breathing found that those with more severe apnea suffer postural stability and are at increased risk for falls. The authors concluded, “Including postural stability assessments in the clinical practice for OSA [obstructive sleep apnea] may help addressing workplace accidents or tendency to fall.”