Whiplash Causes Neck Pain And Other Disorders …
The term “whiplash,” used to describe an injury mechanism of sudden hyperextension (backward motion) followed by hyperflexion (forward motion) of the neck. The injury mechanism is commonly seen in sports and auto accidents. Often, no objective signs of damage to the neck are visible on cervical spine x-rays and no clinical signs of nerve damage are found and it is termed neck sprain or strain injury. A significant proportion of the injured suffer long-lasting or chronic symptoms, and some are disabled for long periods.
The most common symptoms are neck pain, neck stiffness, headache, shoulder pain, back pain, and difficulties with concentration and memory. Dizziness, buzzing in the ears, insomnia, depression, and anxiety also are reported.
Authors of these studies have recommended various types of initial neck pain treatment with analgesics, sedatives, antihistamines, nonsteroid anti-inflammatory drugs, antidepressive drugs, codeine, muscle relaxants, and local anesthetic injections as well as local heat and ice treatment, neck collar immobilization, ultrasound, and physiotherapy. In chronic or long-term cases, surgery and low-energy, high-frequency pulsed electromagnetic therapy have been suggested.
The main event resulting in a whiplash injury is a rear end impact between 2 vehicles. The vehicle that is stationary is impacted, and the forward facing victim typically is not aware of the impact, therefore, is not able to brace herself or himself. Various neck injuries have been clinically documented, mostly at the time of surgery.
These include; interspinous ligament tears, spinous process fractures, disc rupture, endplate avulsion, C2 dens fracture, strain of the occipital and cervical joint complex, ligament flavum rupture, fractures as well as disruptions of facet joints and over-stretching of the front neck muscles. The majority of patients with do not undergo surgery, and, therefore, their soft tissue injuries may remain undetected.

Although the term is widely used, it is not so much a diagnosis as a description of a process of injury. The acute trauma may be categorized as a sprain and/or strain of the neck. Whiplash associated disorders is a collection of signs and symptoms resulting from the injury and often progressing into a chronic condition causing pain and disability for months or years. Common symptoms include, but are not limited to, neck pain, headaches, dizziness, visual disturbances, impaired concentration, and sensory changes in the upper extremities.
It continues to be a burdensome health problem with serious economic consequences. One-third of persons involved in a rear-end motor vehicle collision report neck pain and other symptoms of important severity. In the United States, the economic impact of is estimated at 4.5 billion dollars per year.
After an accident the victim has to cope with a stressful, potentially life-threatening event, in addition to the early physical complaints that result from the accident. The victim may also experience and have to cope with the fear that the complaints may lead to a chronic and invalidating disease. An active coping style is usually considered preferable in this regard and improving active coping strategies is advised as a main treatment goal. During the first weeks of neck complaints after a car accident, those who seek palliative relief of their complaints, experience fear, annoyance, anger or feel inadequate but do not share their concerns or fear with others are at risk of developing chronic or late whiplash syndrome.
Older age, female gender, higher levels of initial neck pain and headache intensity, and initial radicular (nerve) signs/symptoms are predictors of delayed recovery.
- A 2009 study in the Journal of Rehabilitation Medicine indicates that 5 years after injury, persistent symptoms, post-traumatic stress and depression reactions were frequently reported, together with low levels of life satisfaction and reduced social support. Both the total score of pain intensity and of whiplash related symptoms were significantly related to depression, post-traumatic stress scores and psychological factors that also include different aspects of social support many years after a whiplash event requiring additional management in coping with neck pain.
In conclusion, this study demonstrated long-lasting symptoms and psychological consequences, reduced life satisfaction, decline in social support, and difficulties with resuming work. These aspects delineate the complex nature of this injury and should be taken into consideration in the management.
It is unfortunate that it is associated with financial gain and persons are rewarded for faking injury (malingering). This also includes doctors and lawyers (medico-legal system) who pursue unethical methods for financial gain. This is pure corruption, however, it should not reflect the nature of those who are seriously injured. These injuries can often be controversial due to lack of sensitivity of current diagnostic measures, but there is ample scientific evidence relating physical damage to structures responsible for pain and disability.
The structures of the neck which are often involved can be joints, ligaments, discs, arteries, nerves and muscles of the neck.
Facet Joint Pain
The facet joints are frequently a cause of neck pain, especially in those with persistent symptoms. There is ample references regarding facet joint related neck pain leading to diagnostically oriented testing like joint blocks, as well as therapeutic treatment like radiofrequency neurotomy, which is able to alleviate pain in some cases.
 2 joints called facet joints are in-between a pair of neck bones from levels 2 through 7. The joint is covered by a ligament called a joint capsule. A folding on the inner part of the capsule goes in-between the articulations. The capsule of the facet joint cannot prevent excessive motion because it is not rigid.
2 joints called facet joints are in-between a pair of neck bones from levels 2 through 7. The joint is covered by a ligament called a joint capsule. A folding on the inner part of the capsule goes in-between the articulations. The capsule of the facet joint cannot prevent excessive motion because it is not rigid.
The facet joints of the neck are sensitive and may be responsible for wide spread neck pain called a facet syndrome. The motion of the facet joint and capsule during injury forces show 2 types of mechanisms of injury have been proposed – 1) pinching and 2) strain. It is known that the abnormal motion will compress the facet joints, resulting in pinching.
Strain of the facet capsule is well known. Strain levels of 29% to 40% are demonstrated involving the level 6 and C7 joint capsule in whiplash injuries, when strain from normal forward bending are just 5 or 6%. Head turned neck positions have been shown to double the strain in simulations. Incomplete rupturing of the joint capsule is seen with shearing and tensioning as the capsule stretches is another method of damage.
Their induction, persistence, and relationship to joint/capsule mechanics in painful loading supports the facet joint’s involvement as a possible cause of pain.
- A 2022 study in the Annals of Palliative Medicine found cervical facet joint pain is commonly seen after whiplash injury and can be resistant to therapy and medication. In the study corticosteroid injections proved effective for chronic pain when conservative methods failed to produce results.
Ligaments and Disc
Magnetic resonance and autopsy studies of whiplash patients have documented injuries to the neck ligaments and intervertebral discs in addition to the facet joints. Ligament injuries may cause acute neck pain and lead to chronic spinal instability, abnormal muscle response patterns and decreased neck mobility.
Ligaments of the upper cervical spine have unique functional and structural anatomy, predisposing them to partial or complete rupture at low strains. Ligaments provide joint position sense during normal motion and combined with discs provide stability and absorb energy during high speed trauma. The specific function of each cervical ligament and disc in resisting loading is dependent upon its specific anatomical location, orientation, geometry, and unique mechanical properties.
Spinal ligaments and fibers encapsulating the discs can partially or completely rupture when stretched beyond their physiological limit. The related response of the cervical ligaments and discs of the neck have been quantified using a whole cadaveric neck model which replicates muscular forces. During rear impacts with the head facing forward, dynamic strains in the anterior longitudinal ligament and annular disc fibers above physiological levels and increased joint laxity were observed. The C5/C6 disc was found to be at highest risk of injury. The disc injuries occurred at lower impact accelerations during rear impacts compared to frontal impacts.
 Special Pillows Special Pillows |
 Heat Therapy Heat Therapy |
 Cold Therapy Cold Therapy |
Ligament damage may cause instability resulting in loss of motion segment integrity which can be evaluated with flexion/extension x-rays. The AMA Guides to the Evaluation of Permanent Impairment, 5th edition, Nov. 2000, Chapter 15, pages 378-392 place a high impairment rating on loss of motion segment integrity, equating this damage as equal to a vertebra that has a compression fracture greater than 50%. This ligament instability often interferes with normal neck posture, altering the structure of the cervical spine which may lead to chronic health problems.
- Damage to the disc may cause an early onset of degenerative disc disease. A 1991 study published in the journal Injury indicated a significantly higher rate of disc degeneration was found in whiplash patients 10 years after the accident when compared to age matched controls.
It should be noted that a normal MRI study of the neck does not exclude the existence of clinically significant disc disease in the with chronic neck, head or nerve pain. Internal Disc Disruption is a condition where the internal structure of the disc is disrupted, while the external appearance is essentially unchanged. This is often a difficult condition to treat and winds up being a chronic, painful condition, most likely due to persistent inflammation.
Vertebral Artery
The vertebral arteries supply blood to the head, brain, and neck tissues. Changed blood circulation because of spasm and/or constricting of vertebral arterial blood vessels are related to chronic signs and symptoms of headaches, blurry vision, ringing in the ears, lightheadedness, as well as vertigo. Vertebral artery injuries leading to insufficient perfusion to the brainstem and also encompassing tissue might reveal a number of the associated signs and symptoms like headaches and dizziness.
During injury, especially with the head turned and side impacts, stretching of the artery decreases the diameter and may cause vascular compromise. The magnitude, rate, and timing of vertebral artery elongation are sufficient to potentially cause vertebral artery injury.
Dorsal Root and Dorsal Root Ganglion
The dorsal (back) and ventral (front) roots come off the spinal cord and combine to form spinal nerves at each spinal level. Cell bodies of sensory nerves are contained in the dorsal root ganglion, which has been shown to be particularly sensitive to loading. Even slight compression of normal dorsal root ganglia can produce sustained electrical activity and pain. Unlike the nerves which go into the arm, the nerve roots are not enclosed by a thick protective covering, and thus they lack the mechanical strength, potentially exposing nerve roots to increased risk of injury when loaded during injury.

Pressure gradients from blood volume changes related to the spinal canal during rapid forceful motions can place pressure on the ganglia as well as nerve roots and cause symptoms.
Direct injuries to the dorsal root ganglion might make clear a lot of the common signs and symptoms like neck ache, neck related headaches, vertigo, eyesight dysfunction, as well as nerve signs or symptoms within the upper limbs. General sensitivity to pressure and reduced temperature pain thresholds on the skin on the neck may be defined through reduced sensory processing. Greater levels of sensitivity to pain called hyperalgesia, and greater locations of pain referral may also be noted.
Deformation regarding the roots is yet another probable method for creating chronic neck pain. The actual bony openings known as intervertebral foramina alter shape as well as reduce size in the course of excessive neck movements that may constrict nerve roots inside the foramina in the course of injury. It is often noted that a 20% decline in cross sectional area of 4 through 7 foramina levels of the neck with extension and also the foramina at the 5 and 6 level will be reduced up to 1.8 millimeters in the course of simulated rear end collisions. This particular constricting in the foramen in the course of whiplash may possibly constrict the nerve roots as well as ganglia inside the lower cervical vertebrae, especially in people with congenitally small foramen as well as individuals having osteophytes coming from degeneration.
Complaints of neck pain and involvement in one or both arms is often called a cervico-brachial syndrome. Symptoms described as sharp and shooting often result from involvement of the dorsal root ganglion, while irritation of the nerve root often is described as slow in onset and aching in nature.
Findings with nerve irritation is often found when side bending the head towards the painful side and relief when the painful arm is raised above the head. Neck traction is sometimes used to reduce mechanical irritation of the nerve root or dorsal root ganglion.
Muscle
Muscular or myofascial discomfort is a very common. Muscle groups might participate in an indirect function in modulating pain triggered through traumas to other tissues. That is why most injuries are listed as muscle strain.
 Muscle tissue make up most of the neck’s volume level and also the surface muscle groups, like sternocleidomastoid and trapezius, in many cases are suggested as a factor in the pain as well as discomfort related to whiplash injuries. These surface muscle groups connect with the head, shoulder girdle, as well as nuchal ligament yet don’t typically connect immediately to the cervical spinal vertebrae.
Muscle tissue make up most of the neck’s volume level and also the surface muscle groups, like sternocleidomastoid and trapezius, in many cases are suggested as a factor in the pain as well as discomfort related to whiplash injuries. These surface muscle groups connect with the head, shoulder girdle, as well as nuchal ligament yet don’t typically connect immediately to the cervical spinal vertebrae.
Much deeper muscle groups connect to numerous cervical spinal vertebrae. The deepest muscle groups, the multifidus , connect right on the joint capsule of cervical spinal vertebrae and might be related to injuries associated with the capsular ligaments. The majority of neck muscle groups have complicated structures, along with substantial inner tendons as well as the existence and arrangement regarding the inner tendons might be associated to musculotendinous pain.
The primary method regarding neck muscle damage takes place coming from eccentric contractions, which is lengthening in the course of contraction. Computer system models utilizing experimental kinematics involving humans subjected to crashes demonstrate both back and front neck muscle groups encounter active stretching in the course of rear end collisions. With regard to simulated collisions having a velocity change of eight km/h, maximum muscle tissue fascicle strains averaged approximately seven to fifteen percent in the sternocleidomastoid and also 21 to 50 percent within the rear muscle groups like the semispinalis capitis. These types of strains surpassed all those demonstrated to trigger muscular injury (5 to 20 percent) in research laboratory tests, therefore, acute neck muscle tissue injuries can happen in the course of rear end collisions.
Neck muscles most likely communicate with additional anatomical locations associated with whiplash injuries in 3 ways: (one) neck muscle groups connect specifically to the facet joint capsule, that is suggested as a factor in persistent pain right after rearend collisions; (two) neck muscular activation in a roundabout way impacts the forces and strains within additional anatomical sites; and (three) modified neuromuscular command may well bring about persistent pain coming from increased as well as improper muscular activation.
Neck muscular activation additionally impacts tissue loads by means of raising intervertebral pressure as well as modifying usual movement. Due to the fact neck muscle groups tend to be oriented mainly down and up, their particular activation generates axial pressure involving the cervical spinal column, raising loads in the intervertebral discs as well as facet joints. Muscular activation additionally has an effect on the movement reaction associated with the neck and head, therefore loading and also strain thresholds regarding injuries might be surpassed within various other structures like ligaments, discs and also facet joints.
The relationship involving muscle groups and nerves (neuromuscular control) may be additionally associated with persistent pain. A lack of ability to relax following physical exercise as well as increased activation tend to be related to neck pain, plus calming specific neck muscle tissues with botulinum toxins enhances flexibility as well as decreases pain in these sufferers. This implies that pain as well as elevated muscle activity might enhance one another. It continues to be uncertain whether or not muscular dysfunction can be a trigger (resulting in harm to additional structures) or influence (because of disuse or avoiding pain ) regarding discomfort or even just a related connection.
MRI studies have indicated significant changes to the structure of neck muscles in sufferers of persistent symptoms. This type of fatty degeneration of the neck muscles are postulated to be the result of local structural damage, a nerve injury, or a generalized disuse phenomenon.
- In a 2020 study in the journal PLoS One the authors studied acute whiplash patients and compared MRI and CT muscle attenuation values and found they were significantly correlated to muscle fat infiltration. Lower attenuation of the muscles in the deep cervical extensors was seen in the severe group early. However, on MRI at 1 year, fat infiltration was significantly higher in the severe group. They concluded that deep muscle fat infiltration is related to muscle health and looks unique to those at risk of and eventually transitioning to chronic pain and disability.
- A 2020 study in the American Journal of Neuroradiology used functional MRI which measures brain activity and found a correlation between between brain network structure and infiltration of muscle fat. Lower network modularity was associated with larger amounts of cervical muscle fat infiltration.
Some gentle neck exercises may be beneficial to help prevent chronic whiplash.
Studies indicate that upper limb pain and altered sensations may arise from hypersensitivity to pain in nerve tissue. Neck rotation (turning head to the right and left) addresses this involvement by mobilizing the nerve structures on the opposite side to which the neck is turned. This can help to prevent scar tissue from forming adhesions that may later cause dysfunction.

Rotation avoids compression stress caused by flexion (bending head forward) and lateral flexion (bending ear toward the shoulder). This mobilization may also help to increase microvascular blood flow caused by compression. Self-mobilization should begin as soon as possible when there are no major complications. The emphasis should be on frequently repeated neck rotation. Patients may perform gentle, small rotational movements of the neck, first in one direction, then the other. The movements should be repeated 10 times in each direction every waking hour.
The movements should be performed up to a maximum comfortable range. Perform these home neck exercises in the sitting position if symptoms are not too severe. The exercises can be done while lying on the back (unloaded supine position) if the sitting position is too painful. In the event of an increase of symptoms, adjust by either reducing the amount of rotation – amplitude of the movements, by reducing the number of movements, or both. The exercises should not cause an increase in pain.
- A 2015 study in the European Journal Of Pain examined factors related to the reduction of disability & pain in chronic whiplash patients, finding that specific neck exercises was the only one that produced consistent results for success in treatment.
Some general advice:
- Findings in the 2008 journal, PLoS Medicine indicate that those with the lowest expectations for recovery after their whiplash injury will have the poorest recovery, and those with the highest expectations will have the best recovery. They also suggest that a patient’s expectations about getting better are as important as his or her physical symptoms.
The authors say that the more we can influence patients to believe they will make a full recovery, the better chance they will have to recover completely. This means that it may be beneficial for healthcare providers to give support and/or education to patients with that increases their positive feelings toward recovery. This can be advanced with education on self management for recovery.
- A 2019 study in the British Journal of Sports Medicine showed that stress reduction (stress inoculation) that is integrated with exercise as opposed to exercise alone for acute whiplash provided better long term outcomes. Early stress symptoms in treatment are signs of poor recovery, therefore, stress reduction or cognitive behavioral therapy can help reduce disability in those displaying symptoms.
Stress reduction is a form of psychological therapy that can reduce fear of motion and anxiety, which can attribute to chronic pain in certain patients. So, it is important to not only relay this information to the therapist/doctor, but to make sure this type of therapy is offered.
I have seen therapists that were very good and some who actually contribute to stress anxiety. I know as a Chiropractor that reassurance and proper education makes a big difference in those that display stress/anxiety, or who are at risk for chronic symptoms. Taking time for this or a proper referral is important.
If you are not being treated in a reassuring and kind manner, and your deepest concerns are not being addressed in a calming manner, you are not in the right place.
After a rear end collision and professional clinical assessment has ruled out any fractures, serious injuries or complicating factors:
- Admit there’s been a physical injury to your neck, however there’s been no critical harm. Following a whiplash injury your neck just isn’t moving and functioning correctly. The joints and muscles happen to be afflicted yet they possess a healthy capacity to restore and repair, which can be aided through activity.
- It ought to improve fast by having an active strategy; there isn’t any reason long-term impairment must occur. Even though signs and symptoms may possibly continue for some time, the actual acute soreness will probably improve inside of a handful of days or perhaps weeks, undoubtedly adequate in order to get on with your life.
- Acknowledge various other signs and symptoms: Headaches, arm soreness, jaw discomfort, as well as lightheadedness are typical and not really reasons for panic.
- Make use of basic analgesic methods; it is really an aid in order to help with earlier activity. Search for a means to relax and do not worry.
- Extended inactivity is actually unhelpful: Staying away from every day activities slows down recovery. A few activities might entail some discomfort, however hurt isn’t the exact same as harm.
- Keeping as active as you possibly can is essential: Continue to keep moving, do not remain in a single position very long, keep moving around before you’ll stiffen up, and do not entirely keep away from things. The majority of every day activities as well as early come back to work are beneficial.
- Exercises are beneficial: Basic shoulder and neck exercises will be effective and safe – stretching out, conditioning as well as co-ordination exercises ought to be done on a regular basis each day; initial tenderness isn’t a cause for worry.
- Emotional aspects (particularly worry and also fear) tend to be risks regarding developing a persistent problem: Do not get worried and do not scared of motion or discomfort activity as well as a optimistic strategy will be the important factors to preventing long-term difficulties. Do not become an avoider.
Lastly, you should make sure your head rests (head restraints) are adjusted properly. Properly adjusted head rests can significantly reduce the level of injury. If you have sustained an injury, don’t think it can’t happen again. Protect your neck by using the right head rest adjustment and because many older head rests are inadequate, you should make sure it is either capable of being adjusted correctly or upgrade.
- A 2019 study in the Clinical Journal of Pain indicates those at risk for chronic neck pain symptoms after whiplash are significantly associated with factors prior to the collision. The authors found pain related diagnoses and medically unexplained symptoms were correlated with neck pain 12 months after the collision.
The authors speculated this may be due to a sensitization process or low threshold for utilizing health care services pre-collision, and that these risk factors were maintained post-collision. The injury triggers preexisting vulnerabilities which complicate recovery and managing chronic symptoms.
- A 2021 study in the European Journal of Pain indicates thermal and widespread mechanical hyperalgesia occur already in the acute phase, but only in eventually non-recovered patients. This indicates altered pain processing and the importance of proper care and rehabilitation in the early acute phase. Hyperalgesia is an exaggerated response to a painful mechanical stimulus like a pin-prick producing prolonged or severe pain. This is a sign that pain pathways are not functioning normally and may be damaged.
- A 2020 study in Musculoskeletal Care highlights some of the concerns in managing whiplash patients. They identified a sense of collaboration, sense of being out of control, and sense of emotional engagement like feelings of uncertainty distress and satisfaction. There was a lack of conceptual clarity related to shared decision making. This study was done using physiotherapists and point to a model of care or consideration long employed by many Chiropractors.

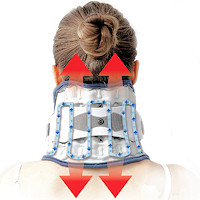 Neck Traction Devices
Neck Traction Devices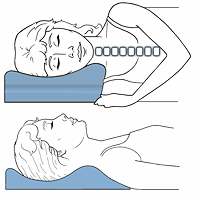 Cervical Pillows
Cervical Pillows Neck Support Collars
Neck Support Collars Muscle Therapy Tools
Muscle Therapy Tools Head Supports
Head Supports Topical Pain Relievers
Topical Pain Relievers TENS Therapy
TENS Therapy Posture Braces
Posture Braces Neck Stabilization
Neck Stabilization Ergonomic Aids
Ergonomic Aids New Mattresses
New Mattresses Relief Supplements
Relief Supplements