A Pinched Nerve In The Neck Can Cause Symptoms Of Pain And Muscle Spasm Due To Arthritis Or Disc Problems
Arm weakness, pinched nerve or cervical radiculopathy usually results from neck arthritis or cervical osteoarthritis, which forms bone spurs and decreases disc height, thus reducing the opening through which a nerve travels causing a pinching of the nerve.
Problems with a herniated disc can place pressure on the nerve along with inflammation which can irritate the nerve. Neck Injury is another cause.
Most commonly, a pinched nerve is experienced in the 4th or 5th decade of life. Typical symptoms of a pinched nerve in the neck may be pain, tingling, numbness or muscle weakness in specific areas related to the path that the nerve travels. The symptoms are sometimes made worse by coughing, sneezing or straining as in moving the bowels. Symptoms usually start at the neck and may travel into the shoulders, arms or fingers depending on how bad the nerve is being pinched.
 You can see in the picture that the nerve in red is being pinched causing pain and inflammation. The disc in light blue is distorted at this level. Normally, the disc is healthy and maintains adequate space for the nerve to pass through. However, a protrusion or herniation of the disc can alter the normal relationship of structures in the neck to cause pinching.
You can see in the picture that the nerve in red is being pinched causing pain and inflammation. The disc in light blue is distorted at this level. Normally, the disc is healthy and maintains adequate space for the nerve to pass through. However, a protrusion or herniation of the disc can alter the normal relationship of structures in the neck to cause pinching.
Similarly, as the nerve travels between the neck bones, a bone spur or degenerated joints from arthritis can also alter the normal relationship and place hard structures on the soft nerve.
Treatment for pinched nerves varies from anti-inflammatory medications, physical therapy, manipulation and sometimes surgery depending on what is pinching the nerve and the extent of any damage.
The dorsal (back) and ventral (front) roots come off the spinal cord and combine to form spinal nerves at each spinal level. Cell bodies of sensory nerves are contained in the dorsal root ganglion, which has been shown to be particularly sensitive to loading. Even slight compression of normal dorsal root ganglia can produce sustained electrical activity and pain. Unlike the nerves which go into the arm, the nerve roots are not enclosed by a thick protective covering, and thus they lack the mechanical strength, potentially exposing nerve roots to increased risk of injury when loaded during an injury like whiplash injury.

Complaints of neck pain and involvement in one or both arms is often called a cervico-brachial syndrome. Symptoms described as sharp and shooting often result from involvement of the dorsal root ganglion, while irritation of the nerve root often is described as slow in onset and aching in nature.
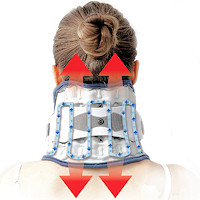
Pinched nerve or radiculopathy findings often increase when side bending the head to the painful side and decrease when the painful arm is raised above the head. Neck traction is a popular method used by professionals to reduce mechanical irritation of the nerve root or dorsal root ganglion.
A Pinched Nerve Can Cause Neck And Scapular Pain Without Arm Or Finger Pain.
 Pain In The Neck or scapular region is one of the most frequent symptoms of a pinched nerve. This neck pain usually is the first sign of radiculopathy and can appear before any symptoms of pain, numbness, or weakness in the arms or fingers. Because typical signs of a pinched nerve in the arm or fingers can be delayed by weeks, this often leads to assumptions that other structures such as muscles are the cause of the neck pain.
Pain In The Neck or scapular region is one of the most frequent symptoms of a pinched nerve. This neck pain usually is the first sign of radiculopathy and can appear before any symptoms of pain, numbness, or weakness in the arms or fingers. Because typical signs of a pinched nerve in the arm or fingers can be delayed by weeks, this often leads to assumptions that other structures such as muscles are the cause of the neck pain.
It has been noted that during diagnostic nerve root injections to determine the involved level, patients perceive only neck or scapular pain first, and arm or finger pain later as the needle is inserted deeper into the nerve root.
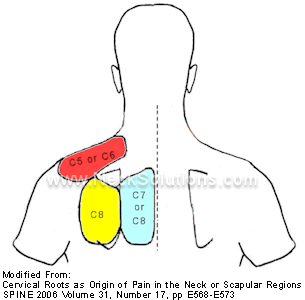
There are usually problems with patients describing the site of pain. Sometimes, the patient cannot reach the area or describe it correctly. In a pain drawing, we can more easily identify the areas of nerve root or radicular involvement, which demonstrates that the site of pain is valuable for determining the localization of the involved nerve.
The most common levels of root involvement are C6 and C7; high cervical radiculopathies (C2-C4) are less common.
It should be noted that the disc space described in diagnostic imaging refers to the nerve root below that level; so that the C5-C6 disc or vertebral pair would place pressure on the C6 nerve root. This is sometimes a cause of confusion as the relationship changes for the lower back or lumbar segments.
Common Symptoms Associated With A Pinched Nerve Are:
C2 – (headaches at the base of the skull & pain at the temples
C3 – (headaches at the base of the skull and/or behind the eyes or ears
C4 – Bottom of the neck and top of shoulders
C5 – Sides of the upper portion of the arms
C6 – Arm pain on the side of the thumb, thumb and/or index finger
C7 – Pain located in the middle fingers
C8 – Last 2 fingers
T1 – Arm pain on the little finger side
 Sensory disturbances with radiculopathy often relate to patterns called dermatomes. The diagram gives a general idea of location, however, it is not always this clear-cut as overlapping can occur.
Sensory disturbances with radiculopathy often relate to patterns called dermatomes. The diagram gives a general idea of location, however, it is not always this clear-cut as overlapping can occur.
Sensory disturbances can be numbness, tingling, decreased or increased sensitivity or itching.
It should be noted that cervical radiculopathy is a neurological condition with signs of loss of neurologic function; a combination of sensory loss, motor loss (weakness) or impaired reflexes in a segmental distribution. The sensory disturbances are what the dermatomes refer to; this does not necessarily mean that pain will follow the path of dermatomes, in fact, pain responses will generally follow similar paths as facet joint pain or pain from the disc, and this distinguishes radicular pain from radiculopathy. For the purpose of this article, we are including both radicular pain and radiculopathy under the term “Pinched nerve”.
Testing for radiculopathy in the clinical setting can be involved, but may lead to a clearer picture. Because the ventral root is sometimes involved causing muscle weakness, testing of muscles for strength is usually performed. Specific muscles are associated with specific nerve roots; deltoid (C5), biceps brachii and extensor carpi radialis longus/brevis (C6), triceps brachii and flexor carpi radialis (C7), abductor pollicus brevis (C8), and dorsal interossei (T1). Muscle strength testing is scored as markedly reduced, reduced, or normal, as compared with the uninvolved arm.
Reflexes are also tested and are associated with specific nerve roots; biceps (C5-C6), brachioradialis (C5-C6), and triceps (C7). These are tested using a standard reflex hammer and each reflex is graded as absent/reduced, normal, or increased, as compared with the uninvolved arm.
Pin-prick sensation testing is performed for the cervical sensory dermatomes (C5-C8) by touching the skin in a key area for each associated sensory level with a paper clip, which is discarded after testing. Each sensory level is graded as reduced, normal, or increased.
A series of 4 provocative tests are often performed with the intent of reproducing or alleviating the symptoms;
- Spurling’s Test – while seated, the clinician bends the head to the involved side and then places downward pressure on top of the head. Sometimes, the head is placed in side bending, rotation and extension to the painful side prior to placing the downward pressure. A positive test is reproduction of the pain or symptoms.
- Shoulder Abduction Test – while seated, the patient is asked to place the hand of the painful side on top of head. A positive test is pain or symptom relief or reduction.
- Neck Distraction Test – while lying on the back, the clinician grasps the chin and the back of the head and pulls away from the patient. A positive test is pain or symptom relief or reduction.
- Upper Limb Tension Test – while lying on back, the clinician puts the arm through a series of motions along with neck side bending to tension the nerve. Positive test is reproduction of symptoms at various stages.
Range of neck motion is also recorded. This is sometimes noted “by eye” or specific methods using a goniometer may be employed.
Additional testing can include x-rays – particularly oblique views, other radiological tests, such as MRI, and more invasive studies such as CT myelography, needle electromyography and nerve conduction studies.
What Can Be Done For A Pinched Nerve?
Combined neck and arm pain are much more disabling than either symptom alone. Patients younger than 40-60 are more affected by these symptoms than patients older than 60 years. As neck and arm pain symptom duration increases, a negative impact on mental health is observed, although chronic symptoms usually do not affect overall physical health. Patients with a significant component of neck pain in conjunction with cervical radiculopathy should be considered the most affected of all.
Prompt treatment may help avoid the harmful effects of chronic symptoms on mental functioning, especially among younger patients who are usually found to be more impacted by these symptoms. Younger patients are generally healthier and more active; symptoms that impair activities have a much greater impact on a younger, healthier population who are more likely to care for children and/or have a job. In addition, younger patients have greater expectations of their physical capabilities than older individuals.
A recent onset of a pinched nerve (acute cervical radiculopathy) generally has a self-limited clinical course, with up to a 75% rate of spontaneous improvement. Thus, nonsurgical treatment is the appropriate initial approach for most patients. When nonsurgical treatment fails to relieve symptoms or if a significant neurologic deficit exists, surgical decompression may be necessary.
Immobilization of the neck with stabilizing cervical collars or soft, but supportive neck braces is thought to diminish inflammation around an irritated nerve root and may also diminish muscle spasms. Alternatively, the warmth provided by wearing the collar may be therapeutic. Traction may help to separate the spinal bones to relieve compression or pinching on the nerve. Neck exercises may be helpful along with moist heat and a good neck pillow as a part of posture modification.
Manipulation is scorned by many medical practitioners. Many in opposition fail to recognize chiropractors are heterogeneous in technique selection and assume all use the same methods and apply the same philosophical concepts. I am not personally aware of any Chiropractor who indiscriminately manipulate a patients neck without concern to any complicating factors which might alter clinical reasoning for technique selection or therapeutic approach. I have personally treated radiculopathy cases with good results and would not hesitate to receive such adjustments myself. Standard technique using a gentle approach is appropriate along with distractive or low force techniques may provide relief and ultimately alter a course of addiction to drugs or surgical intervention.
Nonsteroidal anti-inflammatory drugs (NSAIDs) may provide relief. A patient on long-term NSAID therapy should be monitored for potential liver, kidney, and gastrointestinal toxicity. Narcotic analgesics may be necessary for symptom relief in the early, severe stages of cervical radiculopathy. Because of their addictive potential, however, narcotics are not ideal for the long-term treatment of most patients. In general, narcotics should be used as breakthrough supplements to NSAIDs or in patients who cannot tolerate NSAIDs. The patient should be weaned off the narcotic as soon as possible. Muscle relaxants also may provide symptomatic relief as a means of decreasing narcotic requirements.
Oral corticosteroids are commonly prescribed and there is evidence to suggest they are effective in diminishing acute radicular pain. Methylprednisolone is often prescribed as a prepackaged dose pack that tapers from 24 to 0 mg over 7 days. I found this to be effective for a very painful herniated disc causing a pinched nerve with radiculopathy in my neck.
Spinal steroid injections and nerve root blocks are also used in the nonsurgical management of radiculopathy. Rare complications of cervical injections include dural puncture, meningitis, epidural abscess, intraocular hemorrhage, adrenocortical suppression, epidural hematoma, and root or spinal cord injury.
It is not possible at the start of symptoms to predict whether a given patient will respond well to nonsurgical treatment with a pinched nerve. In the absence of severe or progressive neurologic problems, nonsurgical treatment should be attempted for most patients with cervical radiculopathy. Many forms of nonsurgical management are thought to provide at least some short-term pain reduction. For the patient with progressive neurologic dysfunction or the patient who does not show improvement despite time and nonsurgical neck pain treatment, surgical management does provide good results.



 Neck Traction Devices
Neck Traction Devices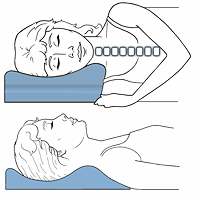 Cervical Pillows
Cervical Pillows Neck Support Collars
Neck Support Collars Muscle Therapy Tools
Muscle Therapy Tools Special Pillows
Special Pillows Topical Pain Relievers
Topical Pain Relievers TENS Therapy
TENS Therapy Heat Therapy
Heat Therapy Cold Therapy
Cold Therapy